Mortality during or shortly after Curative-Intent Radio-(Chemo-)Therapy
Sebastian M. Christ,
Switzerland
PD-0808
Abstract
Mortality during or shortly after Curative-Intent Radio-(Chemo-)Therapy
Authors: Sebastian M. Christ1, Jonas Willmann1, Philip Heesen2, Anja Kühnis1, Maiwand Ahmadsei1, Stephanie Tanadini-Lang1, David Blum3, Panagiotis Balermpas1, Matthias Guckenberger1, Caroline Hertler3, Nicolaus Andratschke1
1University Hospital Zurich, Department of Radiation Oncology, Zurich, Switzerland; 2University of Zurich, Faculty of Medicine, Zurich, Switzerland; 3University Hospital Zurich, Competence Center Palliative Care, Department of Radiation Oncology, Zurich, Switzerland
Show Affiliations
Hide Affiliations
Purpose or Objective
Modern oncological care needs to carefully balance risks and benefits for patients. While often curative, definitive surgical, oncological and radio-oncological treatment may result in significant morbidity and acute mortality, especially in patients with relevant comorbidities. Mortality during or shortly after treatment, often termed “peri-RT mortality”, in patients undergoing curative-intent radio-(chemo)-therapy has not been studied systematically. We therefore analyzed mortality during or shortly after curative-intent radio-(chemo-)therapy at the Comprehensive Cancer Center Zurich (CCCZ).
Material and Methods
The institutional record was screened for all patients who received curative-intent radio-(chemo-)therapy between January 2012 and December 2021 at CCCZ and deceased during or within 30 days after radiotherapy completion/end. Curative therapy was defined as curative-intent as per the treating radiation oncologists, with prescribed dosage EQD2≥50Gy for radiotherapy alone, EQD2≥40Gy for radiochemotherapies and even lower cut-offs for lymphoma patients. Cases of intra- or extracranial local ablative treatments to metastatic disease were excluded. Data on demographics, disease and treatment parameters were assembled and assessed.
Results
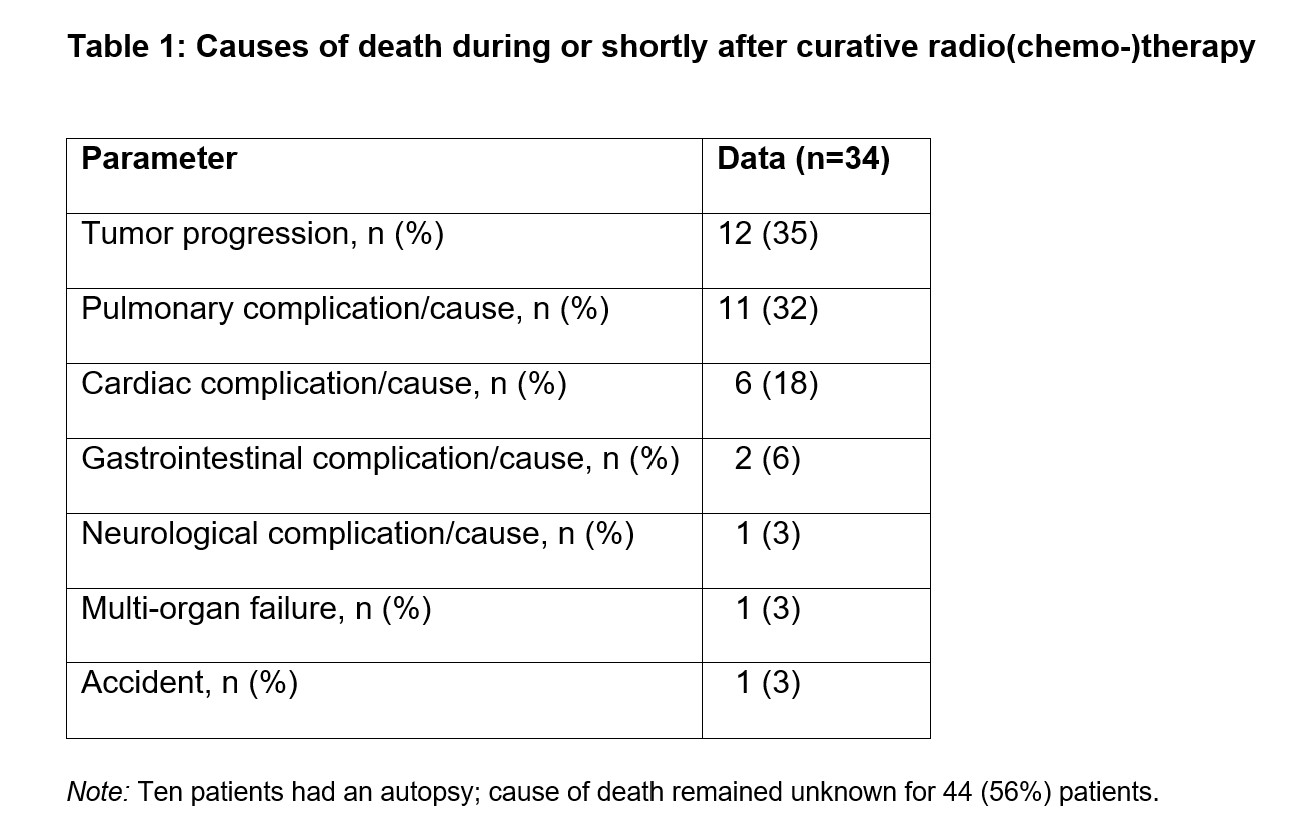
From January 2012 to December 2021, 15,255 radiotherapy courses were delivered at CCCZ, of which 8,515 (56%) treatments were performed with curative-intent. Dur-ing or within 30 days after radio-(chemo-)therapy completion, 78 patients had died, which represents 0.5% and 0.9% of all radiotherapy courses and of all curative-intent radiotherapies at CCCZ, respectively. Their median age was 70 (IQR, 62–78) years, and 36% (28/78) were female. Median pre-therapeutic Eastern Cooperative Oncology Group (ECOG) was 1 (IQR, 0–2) and Charlson-Comorbidity-Index (CCI) was 3+ (IQR, 2–3+) among patients with a well-documented performance (68/78; 87%) and comorbidity status (78/78; 100%), respectively. The most common primary malignancies were head and neck cancer (33/78; 42%), lung cancer (incl. small cell and non-small cell lung cancer; 14/78; 18%), and central nervous system tumors (13/78; 17%). Therapeutic regimen consisted of radiochemotherapy in 32 (41%) and radiotherapy alone in 46 (59%) patients, respectively. Median prescribed dose was 65 (IQR, 50–70) Gy. Median number of days between treatment start and death was 8 days (IQR, 2–20); two patients died before the first fraction. Among patients with known cause of death (34/78; 44%), tumor progression (12/34; 35%) and pulmonary complications/causes (11/34; 35%) were most common (Table 1).
Conclusion
During the last decade, 0.9% of all patients who received a curative-intent radio-(chemo-)therapy at CCCZ deceased during or within 30 days of therapy completion, which indicates that risks and benefits were carefully weighed by treating physicians. Future research should aim to identify predictors for peri-RT mortality and to develop mitigation strategies.