No changes in pulmonary function by spirometry after Stereotactic Body Radiotherapy in lung lesions
Abraham Andre Arturo Geng Cahuayme,
Spain
PD-0157
Abstract
No changes in pulmonary function by spirometry after Stereotactic Body Radiotherapy in lung lesions
Authors: Abraham Andre Arturo Geng Cahuayme1, Alexandra Giraldo Marín2, Mónica Ramos Albiac2, Josep Garre Cristau2, Enar Recalde Vizcay2, Jordi Giralt López de Sagredo2
1Vall d'Hebron University Hospital, Radiation Oncology , Barcelona, Spain; 2Vall d'Hebron University Hospital, Radiation Oncology, Barcelona, Spain
Show Affiliations
Hide Affiliations
Purpose or Objective
To evaluate changes in pulmonary function by spirometry after SBRT in lung lesions treated with radical intention over 2-years follow-up in patients without radiological progression or death.
Material and Methods
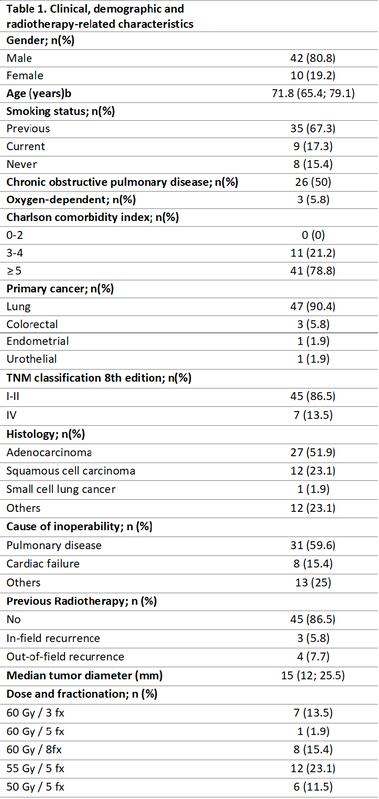
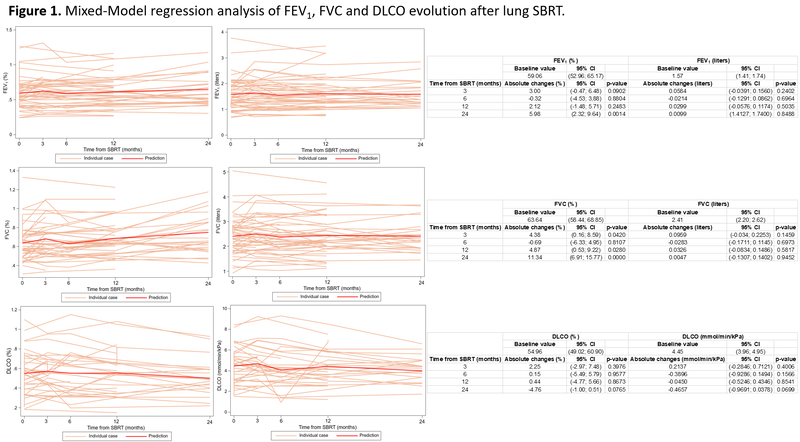
A single-center, retrospective study was performed in a Spanish tertiary hospital that analyzed pulmonary function after lung SBRT from January 1, 2015, to January 31, 2020. Patients included were ≥18 years of age and KPS>70, with primary lung cancer or lung metastases smaller than 5cm. Patients were eligible for radiotherapy on a tumor board if they were considered to be inoperable for medical reasons, or refused to undergo surgery. Patients were excluded from the analysis if they had interstitial lung disease or active lower respiratory infection. All patients included had baseline spirometry and at least 2 spirometries during the follow-up. Mixed-effects model were used to evaluate changes in FEV1, FVC, and DLCO at 3, 6, 12, and 24 months after SBRT.
Results
Fifty-two lung lesions underwent SBRT. The clinical, demographic, and radiotherapy-related characteristics included in the present study are shown in Table 1. Mixed-model regression analysis was performed to predict changes in values of pulmonary functions tests such as FEV1, FVC, and DLCO which is represented in figure 1. No significant differences were observed during the first year in both liters and the percentage of predicted in FEV1 evolution. A gain of 5.9% [95% CI, 2.3; 9.6 percent (p=0.0014)] was beheld after 24 months post-SBRT. Although, there was no significant difference when FEV1 was analyzed in liters 24 months post SBRT (fig 1A-B). Significant differences were observed with increasing FVC in percentage at 3, 12, and 24 months after SBRT. However, no significant differences were found in FVC evolution according to liters during the first two years post-treatment (fig 1C-D). Finally, no differences were reported when analyzing DLCO evolution according to percentage and ml/min/kPa (fig 1E-F).
Conclusion
In our study, we could conclude SBRT in primary lung tumors or pulmonary metastases does not negatively influence pulmonary function assessed by spirometry at least in the first two years after treatment.