Radiation induced lymphopenia, its effect on pathologic regression and prognosis in LA lung cancer
PD-0153
Abstract
Radiation induced lymphopenia, its effect on pathologic regression and prognosis in LA lung cancer
Authors: sarit appel1, Jair Bar2, Yaacov Richard Lawrence1, Demian Urban2, Zvi Symon1, Jeffry Goldstein3, Shira Felder1
1Sheba Medical Center, Radiation Oncology, Ramat Gan, Israel; 2Sheba Medical Center, Oncology, Ramat Gan, Israel; 3Sourasky Medical Center, Radiation Oncology, Tel Aviv, Israel
Show Affiliations
Hide Affiliations
Purpose or Objective
Previous studies associated lymphopenia following neo-adjuvant chemoradiation (n-CRT) with adverse outcomes. We hypothesized that lymphopenia following n-CRT and surgery will correlate with decreased tumor regression and poor prognosis in locally advanced non-small cell lung cancer (LA-NSCLC).
Material and Methods
Patient characteristics, treatment variables and lymphocyte nadir were extracted for analysis from an IRB approved database of patients with LA-NSCLC treated with n-CRT followed by surgery. Lymphopenia, graded according to CTCAEv5, was analyzed as continuous and categoric variables (grade 0-2 vs. grade 3-4). Primary endpoints based on surgical specimens were major pathologic regression (MPR), pathologic complete response (pCR), and mean residual tumor cells (MRTC). Secondary endpoints were local control (LC), disease free (DFS) and overall survival (OS). Logistic regression, spearman correlation and Kaplan Meir analysis were used to identify effects of lymphopenia on endpoints
Results
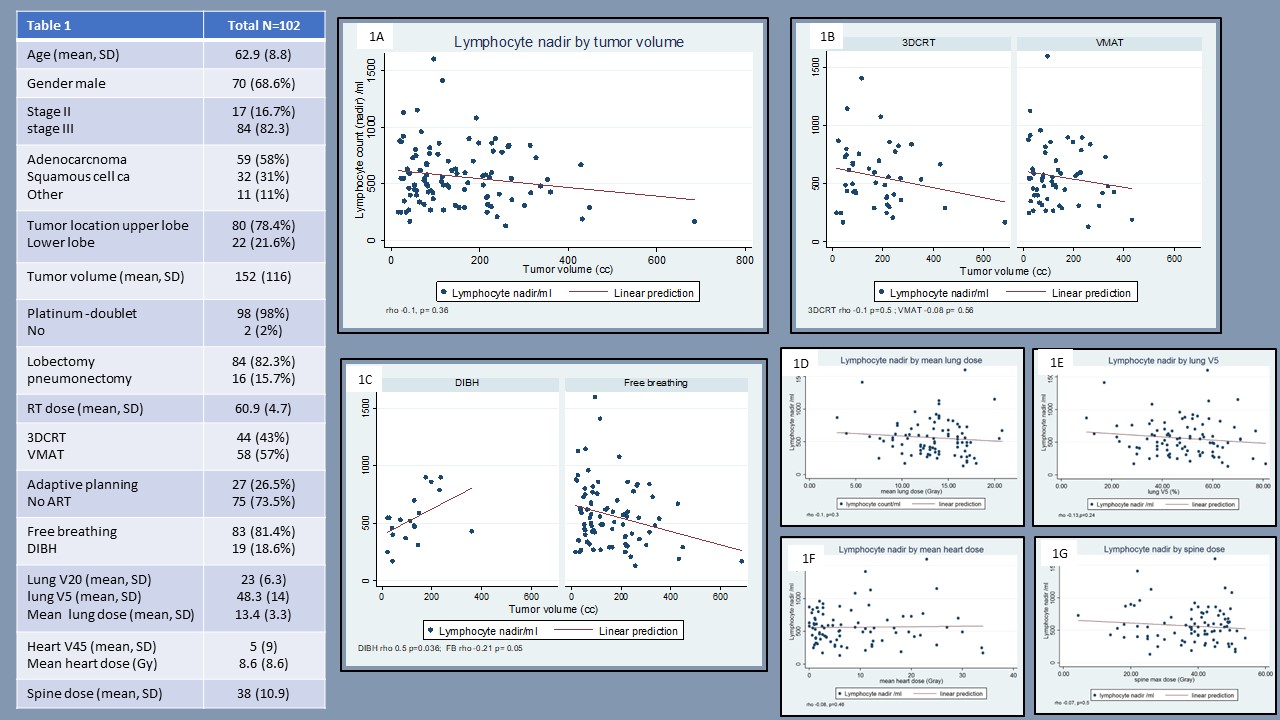
Database review identified 102 patients eligible for inclusion. Patient and treatment characteristics are presented in table 1.
Median lymphocyte nadir was 535 (IQR 380-730) categorized as grade 2 (n=37, 36%), grade 3 (n=42, 41%) and grade 4 (n=4, 4%) and occurred during the final 2-weeks of n-CRT. Although lymphocyte count recovered before surgery, rebound lymphopenia (median 400 IQR 300-540) occurred upon surgery.
Spearman analysis suggested lymphocyte count decreased as tumor volume increased (rho -0.1, p=0.36) and (fig.1A). Use of either VMAT or 3DCRT techniques did not change this relationship (fig. 1B). Yet, use of deep inspiratory breath hold (DIBH) technique changed the effect of tumor volume (fig.1C p=0.05). No other variables correlated with lymphopenia, including dosimetric variables (fig.1D-G).
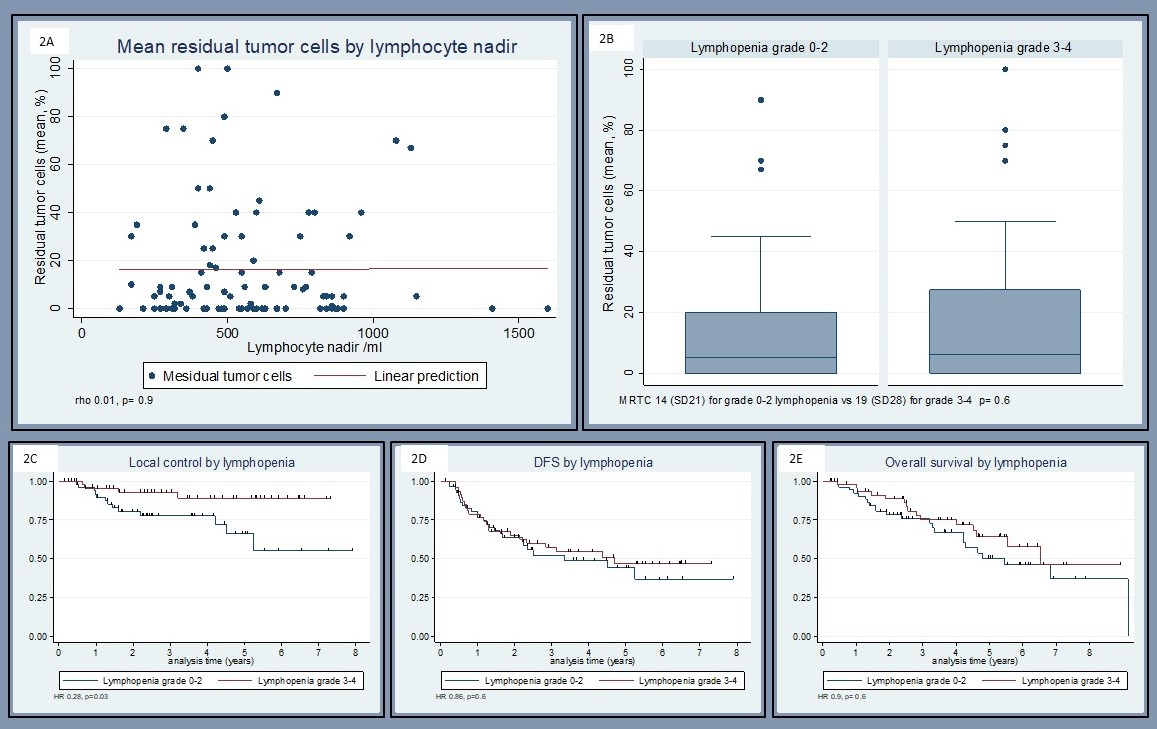
MPR was recorded in 31/48 (64.6%) with lymphopenia grade ≥3 vs. 36/54 (66.6%) for grade ≤2 (OR 1.1 p=0.82). PCR was recorded 18/48 (37.5%) with lymphopenia grade ≥3 vs. 20/54 (37%) for grade ≤2 (OR 1.02, p=0.96). Mean residual tumor cells did not correlate with lymphocyte count (rho 0.01, p=0.9). The MRTC was 14% (SD21) for grade 0-2 vs. 19% (SD28) for grade 3-4 lymphopenia p=0.6 (fig 2A-B).
Although LC was improved with lymphopenia (HR 0.28, p=0.03), DFS (HR 0.86, p=0.6) and OS (HR 0.9, p=0.6) were unaffected by lymphopenia (fig.1C-E).
Conclusion
Lymphopenia grade ≥3 during n-CRT occurred in 45% of patients, was correlated with tumor volume in treatments delivered in free breathing but not in breath hold. Although lymphocyte count recovered, following surgery, rebounded lymphopenia was observed. Contrary to our hypothesis, lymphopenia during n-CRT did not correlate with pathologic regression and did not impair DFS and OS.