Effects of radiotherapy interruptions in lung cancer disease control: a multicenter study
Elias Gomis Selles,
Spain
PD-0151
Abstract
Effects of radiotherapy interruptions in lung cancer disease control: a multicenter study
Authors: Elias Gomis Selles1, Óscar Muñoz Muñoz1, Blas David Delgado León1, Pablo Jiménez Labaig2, Jon Cacicedo Fernández de Bobadilla2, Pedro Romero Pareja1, Imanol Paguey Garrido1, Sonia Pérez Luque1, Manuel Borrego Reina1, José Luis López Guerra1
1Virgen del Rocio University Hospital, Radiation Oncology, Sevilla, Spain; 2University Hospital Cruces, Radiation Oncology, Bilbao, Spain
Show Affiliations
Hide Affiliations
Purpose or Objective
The evidence about the impact of radiotherapy (RT) interruptions on disease control is scarce and presents biases. The main objective of this study is to assess the impact of RT interruptions on overall survival (OS) and local recurrence-free survival (LRFS) in patients with lung cancer treated with radical intention.
Material and Methods
Retrospective cohort study selecting all patients with lung cancer treated with radical intention with RT in three institutions between October 2008 and August 2021. Exclusion criteria included patients with a lack of information about the reason for interruption or the total dose administered. Log-rank test and Cox regression were employed to analyze OS and LRFS. Chi-square test was used to compare distributions.
Results
A total of 609 patients with lung cancer who received a median of 64Gy were selected. According to the tumor characteristics, most of the patients the most of patients presented non-small cell lung cancer (NSCLC, 85.5%), and stage III (86.0%).
449 patients (74%) discontinued treatment within a median of 2 days (range 1-16). 30% of the days that treatment was interrupted were due to holidays, 12% to toxicity, and 58% to other reasons (breakdowns, maintenance, undetermined). The median of interruptions due to toxicity was 3 days (range 1-16). Fifteen patients (3.3%) had a replanning of their treatment. We did not find a different risk for presenting and interruption in patients who received concomitant chemotherapy (p = 0.63) or with a Karnofsky score higher than 80 (p = 0.78). It was found more interruptions in NSCLC than SCLC (X2 = 1.98; p = 0.001; OR = 1.20).
Patients who discontinued due to toxicity were excluded from survival analysis to avoid potential biases. When comparing patients who prolong their treatment with patients who do not interrupt, we found no significant differences in OS (p = 0.983), neither in LRFS (p = 0.903).
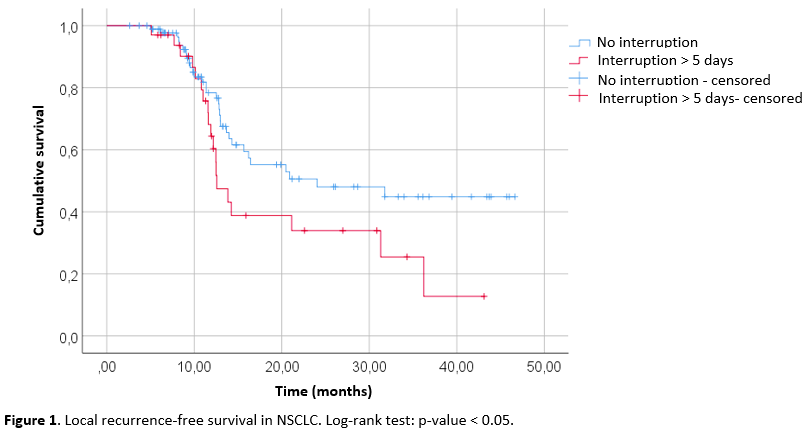
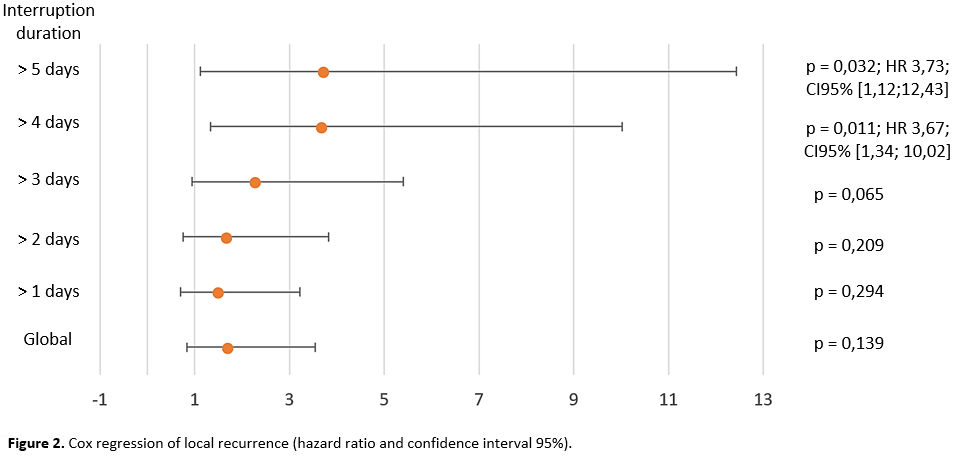
In the subgroup study, during a 4-year follow-up, we found an increased risk of local relapse near to significance in patients with NSCLC who discontinued for more than 5 days (p = 0.052) (Fig. 1). However, we observed a significant increase in the risk of local recurrence in patients with adenocarcinoma histology who discontinued for more than 4 days (HR 3.67; CI95% [1.34; 10.02], p-value = 0.011) (Fig. 2). In SCLC we did not find differences in LRFS (p = 0.20). No differences in the OS or LRFS were found according to histology.
Conclusion
Our data show that only 12% of interruptions in lung cancer were related to toxicity. Moreover, differences according to histologies were found. Our results suggest that patients with NSCLC could experiment more interruptions than SCLC which could impact in prognosis, especially in adenocarcinoma with interruptions for more than 4 days where we found a significant reduction in LRFS. We consider that this subgroup could benefit from compensatory measures. No other alterations in OS or LRFS were identified based on interruptions when we analyzed them according to histology.