Dosimetric consequence of intra-fractional motion for stereotactic treatment of central lung lesions
Simon Nyberg Thomsen,
Denmark
PD-0746
Abstract
Dosimetric consequence of intra-fractional motion for stereotactic treatment of central lung lesions
Authors: Simon Nyberg Thomsen1,2, Ditte Sloth Møller3,4, Marianne Knap5, Tine Bisballe Nyeng4, Lone Hoffmann3,4
1Faculty of Health, Aarhus university, Department of Clinical Medicine, Aarhus, Denmark; 2Aarhus University Hospital, Department of Oncology, Medical Physics, Aarhus , Denmark; 3Faculty of Health Sciences, Aarhus University, Department of Clinical Medicine, Aarhus, Denmark; 4Aarhus University Hospital, Department of Oncology, Medical Physics, Aarhus, Denmark; 5Aarhus University Hospital, Department of Oncology, Aarhus, Denmark
Show Affiliations
Hide Affiliations
Purpose or Objective
Stereotactic radiotherapy (SRT) for small peripheral lung lesions results in high local control rates. However, former SRT trials on centrally located lesions have shown high toxicity levels including grade 5. In the STRICT-lung trial (NCT05354596), central lung lesions are treated with SRT, using an inhomogeneous dose distribution to the target, always favoring rigorous constraints to organs at risk (OAR). The mean dose to the GTV D(GTVmean) is escalated up to 85Gy in 8 fractions, but is limited by the OAR constraints. Due to the proximity to the OAR, this results in a steep dose gradient, very sensitive to intra-fractional shifts. In this study, we present the dosimetric consequences of intra-fractional motion observed for STRICT-lung patients (pts).
Material and Methods
Eighteen pts have been treated in/ad modum the STRICT-lung trial. The PTV margin was 4mm. The pts were set up based on daily cone beam CT (CBCT) soft tissue target match to the planning CT (pCT). After treatment delivery, a second CBCT image was obtained for investigation of intra-fractional target shifts. Retrospectively, the two CBCTs were matched to the pCT on the target and the intra-fractional 3D target shift was calculated.
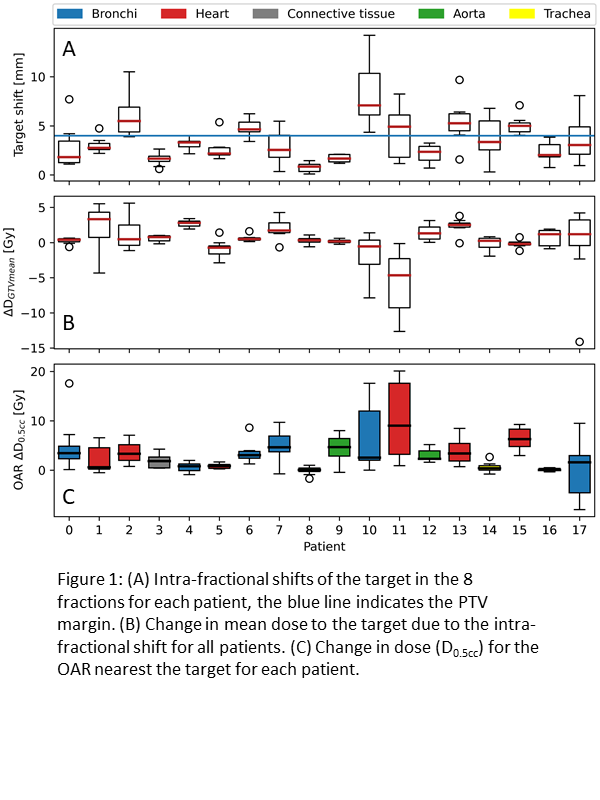
For each fraction, contours delineated on the pCT were deformably transferred to both CBCTs and the dose was calculated based on stoichiometric calibration curves. The difference in D(GTVmean) and dose D(0.5cc) to the OAR closest to the lesion was calculated for all eight fractions and plotted as box plots.
Results
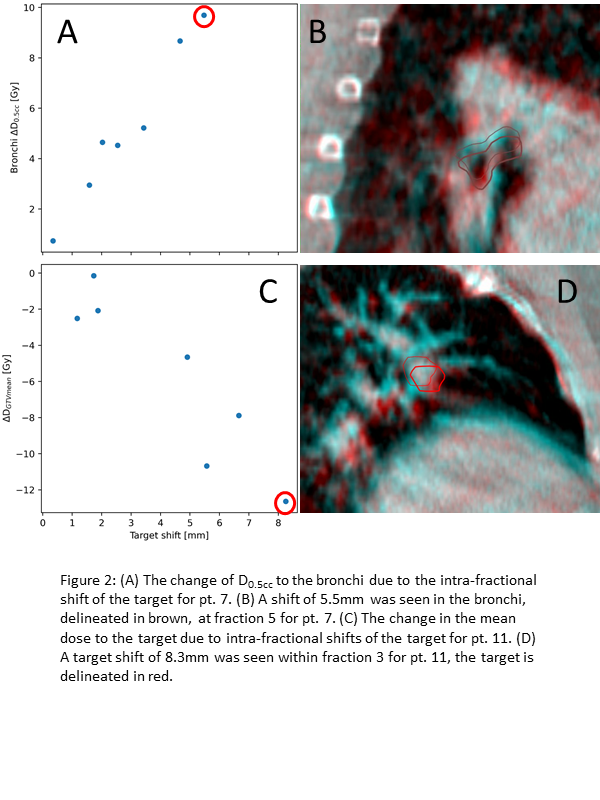
The median [range] target shift was 2.9mm [0.1, 14.2]. A boxplot of the shifts for each pt is shown in Fig 1A, together with the PTV margin. The target shifts were primarily in the cranial and dorsal directions. The median change in D(GTVmean) was 0.44Gy [-14.11, 5.61], meaning that some of the pts received far less target dose than planned due to intra-fractional target shifts (Fig 1B). For most of the pts, the OAR in the closest proximity to the lesion was shifted towards the high-dose region resulting in an increased dose (Fig 1C). Both target shifts and how they influenced the dose to the target and OARs were highly pt -specific and depended on both target location and planned dose distribution. Fig 2 illustrates the dosimetric and geometric shifts for pts 7 and 11. The direction of the shifts seen in these pts is similar to what is observed in most of the other pts. For pt 7 the bronchi move into the high-dose region, while for pt 11 the lesion moves out of the high-dose region resulting in a drop of the D(GTVmean) from 77Gy to 64Gy.
Conclusion
Intra-fractional movements of the target and OAR may result in risk of increased toxicity, and for some pts under-dosage of the target. To ensure the safe delivery of SRT to centrally located lung lesions, it is necessary to monitor and correct for the intra-fractional target shift of the treated pts. It may be necessary to acquire an additional CBCT mid-treatment, to reposition pts with observed large intra-fractional target shifts.