Optical coherence tomography computational model to quantify radiotherapy induced skin effects
PO-1280
Abstract
Optical coherence tomography computational model to quantify radiotherapy induced skin effects
Authors: Meritxell Mollà1, Gabriela Oses2, Gloria Tena3, Marc Combalia3, Andrea Combalia3, Pablo Iglesias4, Beatriz Alejo3, Alba Huguet1, Susana Garrido1, Jordi Solà1, Cristina Carrera3
1Hospital Clínic Barcelona, Radiation Oncology, Barcelona, Spain; 2Hospital Clínic, Radiation Oncology, Barcelona, Spain; 3Hospital Clínic Barcelona, Dermatology, Barcelona, Spain; 4Hospital Clinic Barcelona, Dermatology, Barcelona, Spain
Show Affiliations
Hide Affiliations
Purpose or Objective
Acute radiodermitis remains the most common adverse effect of whole breast radiation therapy (WBRT) in patients with breast cancer (BC). There is currently no objective and reproducible method to measure this effect, nor is there a standardized adjuvant therapy to prevent it. Optical Coherence Tomography (OCT) imaging of skin could be a promising tool in clinical management and research of several skin conditions. The primary objective was to demonstrate skin changes induced by WBRT with OCT scanning. Secondary objectives are to compare radiodermitis grade related to the various radiotherapy (RT) regimes and their impact on quality of life.
Material and Methods
An observational, prospective study of 39 BC patients and candidates to WBRT were grouped by fractionation: 15 fractions (total dose 40.05 Gy) 38.46% of the patients, 20 fractions (total dose 40.05 Gy plus 13.35 Gy to the tumor bed) 35.89% of the patients and 25 fractions (total dose 50 Gy and 57.5 Gy to the tumor bed) 24.64% of the patients. Patients were studied by clinical examination (CTCAE 3.0), quality-of-life questionnaire (EORTC QLQ-C30), and OCT at baseline, the end, and 3 months after completing RT. OCT volumes were processed following an algorithm developed by a biomedical engineer to detect the amount of blood in the sample. Through a series of computer vision techniques, it was possible to extract the vascularized regions, which are represented as red color on top of the skin's structure. General recommendations and a specific hypoallergenic restorative cream were provided to the participants daily use during the RT and for least one month after.
Results
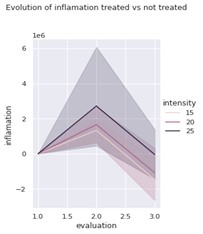
OCT imaging detected a statistically significant increase in inflammation at the end of RT compared to the skin changes for each patient for the irradiated vs. non irradiated breast (p <0.05), and showed decrease in erythema at 3 months (p 0.032) in the irradiated breast (Figure 1). OCT showed quantitative differences with different fractions schemes, with higher intensity changes in vascularization and erythema at 25 fraction regime (Figure 2) The overall tolerance was good, with no differences between groups i.e 30.8% didn’t show radiodermitis, 64.1% radiodermitis G1 and 5.1% G2. The impact on patients' quality of life was low with a total of 53.08% of patients have EORTC QLQ-C30 > 80, and 38.46% between 50 to 80.
Figure 1: Clinical and OCT imaging in baseline (t0), and the end of RT (tF) and at 3 months (t+3)

Figure2: Intensity changes in vascularization in irradiated breast measured by OCT scanning in baseline (t0), and the end of RT (tF) and at 3 months (t+3)
Conclusion
OCT imaging could detect and quantify the effects on microvasculature caused by RT and could represent an advance in the standardization of changes in WBRT. These preliminary results will allow for the design of protocols for measuring and comparing the degree of radiodermitis and the potential benefits of adjuvant therapies.