Is comorbidity associated with interruption of RT treatment in patients with lung cancer?
Golnoosh Motamedi-Ghahfarokhi,
United Kingdom
MO-0474
Abstract
Is comorbidity associated with interruption of RT treatment in patients with lung cancer?
Authors: Golnoosh Motamedi-ghahfarokhi1, Corinne Faivre-Finn1, Marcel Van Herk1, Hitesh Mistry2, Gareth Price3, Azadeh Abravan3
1University of Manchester/The Christie NHS Foundation Trust, Division of Cancer Sciences, School of Medical Sciences, Faculty of Biology, Medicine and Health and Department of Radiotherapy Related Research, Manchester, United Kingdom; 2University of Manchester, Division of Cancer Sciences, School of Medical Sciences, Faculty of Biology, Manchester, United Kingdom; 3The University of Manchester/ The Christie NHS Foundation Trust, Division of Cancer Sciences, School of Medical Sciences, Faculty of Biology, Medicine and Health and Department of Radiotherapy Related Research, Manchester, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Radiotherapy (RT) plays an important role in the management of patients with lung cancer. Many patients present with comorbidities, and the degree to which comorbidity burden affects outcomes after treatment is not fully understood. An important factor influencing outcomes is the timely completion of treatment. This study presents comorbidity prevalence in a cohort of patients with non-small cell lung cancer (NSCLC) and investigates if baseline comorbidities are associated with treatment interruption.
Material and Methods
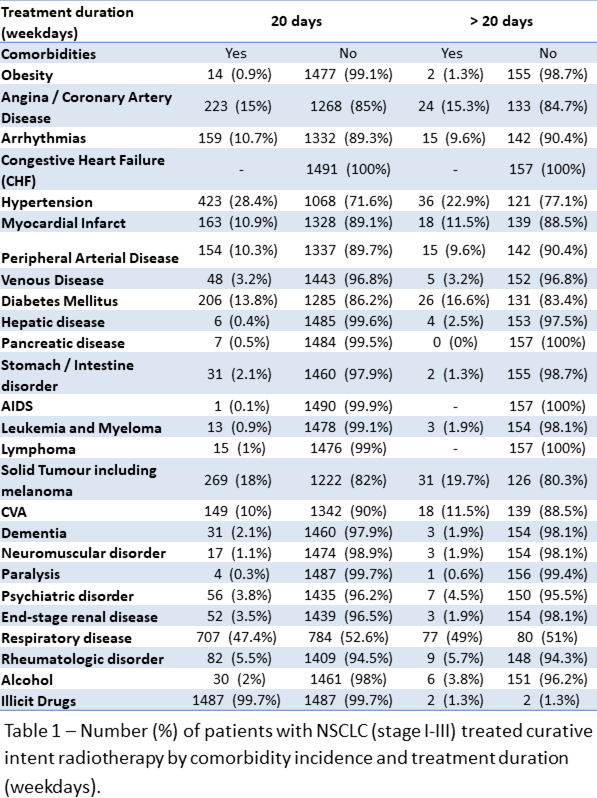
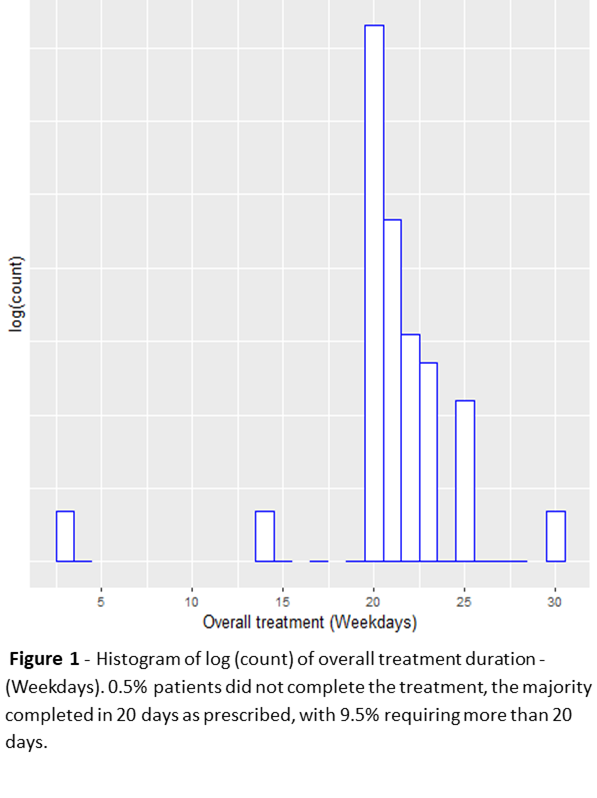
Data from 1,656 stage I-III NSCLC patients treated with curative-intent RT (55 Gy in 20 fractions, +/- sequential chemotherapy) between January 2013 and June 2022 with available Adult Co-Morbidity Evaluation (ACE-27) from a single institute were collected. RT was given to patients on weekdays over four weeks. Overall treatment duration (days) was defined as the number of weekdays from treatment initiation to last fraction received. Comorbidities were collected at diagnosis using ACE-27 values and were considered as a binary variables (with/without comorbidity). Total comorbidity burden was categorised as none, one, two, and more than two comorbidities. The association of each comorbidity and the total number of comorbidities with overall treatment duration was assessed via multivariable linear regression.
Results
1,491 patients completed treatment within 20 days, 157 took more than 20 days and 8 patients never completed the treatment due to death that were excluded from analysis (Figure 1). Cardiovascular (32%), respiratory (29%) and endocrine (8%) conditions were the most common comorbidities (Table 1). After adjusting for age, sex, T stage, N stage, performance status, gross tumour volume (GTV), only obesity (1%) was found to be associated with an increase in treatment duration by an average of 1 day (p = 0.011). Regarding the total number of comorbidities, overall treatment duration for patients with one (p = 0.017), two (p = 0.003), and more than two (p = 0.022) comorbidities increased by an average of 0.2, 0.3, and 0.2 days respectively (but not by a clinically relevant amount) than those that had no comorbidities.
Conclusion
In this cohort of stage I-III NSCLC patients treated with curative intent radiotherapy +/- sequential chemotherapy there is little evidence of any association between comorbidity burden and an increase in treatment duration that could signify treatment interruption. These data suggest that comorbidities do not have a significant impact on radiotherapy interruption.