MRI-based inter- and intra-fraction motion of the spleen/pancreatic tail in neuroblastoma patients
Fasco van Ommen,
The Netherlands
MO-0386
Abstract
MRI-based inter- and intra-fraction motion of the spleen/pancreatic tail in neuroblastoma patients
Authors: Fasco van Ommen1, Gaelle A.T. le Quellenec1, Mirjam E. Willemsen-Bosman1, Max M. van Noesel2, Enrica Seravalli1, Petra S. Kroon1, Geert O.R. Janssens1
1University Medical Center Utrecht, Radiotherapy, Utrecht, The Netherlands; 2 Princess Máxima Center for Pediatric Oncology, Solid Tumors, Utrecht, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
In state-of-the-art radiotherapy treatment planning, dose constraints to the spleen/pancreatic tail in pediatric patients with neuroblastoma and renal tumors are applied. An analysis of MRI-based inter- and intrafraction motion of the spleen/pancreatic tail is performed to estimate the potential dose reduction using an adaptive MR-linac (MRL) workflow.
Material and Methods
Ten consecutive pediatric patients (median age 3.4 years, range 1 – 9 years) with a neuroblastoma originating from the upper abdomen, previously irradiated with photons (21.6 Gy; 12 fractions of 1.8 Gy) at our department, were retrospectively evaluated for inter- and intra-fraction motion of the spleen/pancreatic tail. In addition to an MRI in radiotherapy position, all patients underwent ≥3 repeat MRIs. The MRI sessions consisted of a T2- and T1-weighted ± gadolinium MRI. All images were rigidly registered, based on a mutual information method, on the spine to the planning CT (pCT). For interfraction motion analysis, the spleen/pancreatic tail were delineated on all MRIs and compared to their position on the pCT. For intrafraction motion analysis, the position of both organs was compared to the first acquired MRI of each day. In addition, the dose distribution of the clinical radiation plan was used to estimate the mean dose (Dmean) to both spleen/pancreatic tail for the different time points.
Results
For the 10 patients, the mean interfraction motion of the pancreatic tail (X: 1.1 ± 3.8, Y: -1.4 ± 4.4 and Z: -4.3 ± 6.6 mm) and spleen (X: 1.8 ± 1.8, Y: -1.3 ± 5.3 and Z: -0.3 ± 5.8 mm) was larger than the motion of these organs due to respiratory motion and was characterized by the large standard deviations of movements (interfraction motion (mm) is shown in Figure 1A and 2A). The mean intrafraction motion was smaller, but also showed large standard deviations (pancreatic tail; X: 0.5 ± 2.0, Y: 0.3 ± 3.1 and Z: 1.4 ± 5.2 mm; spleen; X: 0.9 ± 1.9, Y: -0.5 ± 3.7 and Z: 1.3 ± 5.4 mm). The Dmean of the pancreatic tail and spleen varied between -5.8 to +3.3 Gy and -3.1 to +1.8 Gy (Figure 1B and 2B).
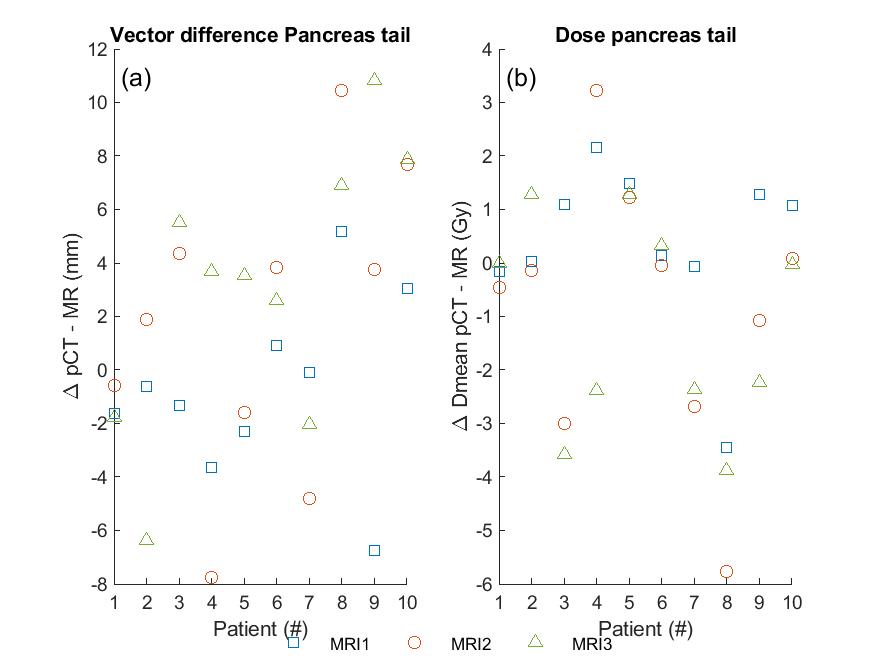
Figure 1: Pancreas tail dose difference (Gy) between pCT and MRI (a) and the motion in mm of the pancreas tail (b). It shows that when the pancreas tail moves towards the target, an increase in dose is observed.

Figure 2: Spleen dose difference (Gy) between pCT and MRI (a) and the motion in mm of the spleen (b). It shows that when the spleen moves towards the target, a minimal increase in dose is observed.
Conclusion
A large individual spread in inter- and intrafraction motion for the spleen/pancreas tail is observed in pediatric patients with neuroblastoma, potentially resulting in higher doses to these OARs. Daily adaptive MR-guided radiotherapy might be able to substantially reduce the dose to the spleen/pancreatic tail, but this requires more evaluation.