SBRT vs 3D-CRT FOR OLIGOMETASTATIC BONE NSCLC
PO-1254
Abstract
SBRT vs 3D-CRT FOR OLIGOMETASTATIC BONE NSCLC
Authors: Giulia Marvaso1, Ekaterina Milovanova2, Riccardo Santamaria1, Stefania Volpe1, Giulia Corrao1, Mattia Zaffaroni3, Matteo Pepa3, Maria Giulia Vincini3, Oriana D'Ecclesiis4, Sara Gandini4, Gaia Piperno3, Annamaria Ferrari3, Roberto Orecchia5, Barbara Alicja Jereczek-Fossa1
1IEO, European Institute of Oncology IRCCS; University of Milan, Division of Radiation Oncology; Department of Oncology and Hematoncology, Milan, Italy; 2University of Milan, Department of Oncology and Hematoncology, Milan, Italy; 3IEO, European Institute of Oncology IRCCS, Division of Radiation Oncology, Milan, Italy; 4IEO, European Institute of Oncology IRCCS, Department of Experimental Oncology, Milan, Italy; 5IEO, European Institute of Oncology IRCCS, Scientific Directorate, Milan, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
Bone
is one of the most common and earlier site of metastases from non-small cell lung
cancer (NSCLC), occurring in about 10% - 35% of cases during the course of disease.The current standard of
care for patients with symptomatic bone metastases is a low total dose of radiation
delivered with conventional external beam
RT. The aim of this
retrospective analysis is to explore whether SBRT could improve the local
control and the complete response rate for pain compared with conventional
external beam RT in oligometastatic bone NSCLC.
Material and Methods
Patients
with histologically confirmed NSCLC and oligometastatic disease (number of metastases ≤ 5),
painful bone metastases (according to the Numerical Rating Scale [NRS]), Karnofsky
Performance Status scores ≥80 and treated with SBRT vs 3D-CRT between January 2015 and December 2020 with a minimum follow-up
of 3 months were included in the study. The
primary endpoint was local control measured by radiological and
clinical response. Secondary endpoints
included complete clinical
response rates for pain, QoL and adverse events (including rates or
fracture).
Results
A total of 122 patients met the inclusion criteria either in 3D-CRT group (n=59), SBRT group (n=62) or both (n=1). Seventy
percent of the patients presented a number of lesions < 3, in 50 patients (41%)
all lesions were treated. Median total dose over all treatment techniques was
24 Gy (IQR 20-25) in a median number of fraction of 5. Clinical characteristics
of the patients and clinical and radiological rate of response are summarize in
Table 1.
After a median follow-up of 3 months, treatment
with SBRT lowers the risk of disease progression by 75% (OR=0.25, CI 95%
(0.05-0.90)). However there appears to be no significant association between
technique and radiological response at multivariate analysis (p= .07).
For patients
with a number of metastases ≥ 3 (30%), SBRT treatment lowers the risk of
disease progression by 88% (p= .01). In addition, those who have a total number
of lesions ≥3 have a 1.9 times higher risk of disease progression (OR=2.91
(0.83-10.59)).
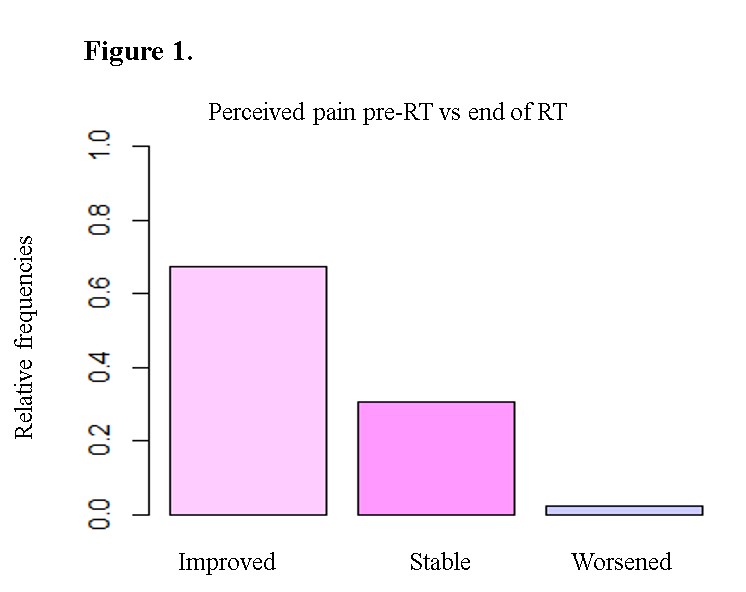
A significant association
between technique and clinical response was observed (p =.02). In fact, 34% of patients (n=22) in SBRT group showed
complete clinical response in comparison to 15% (n=15) in 3D-CRT group. Furthermore,
there association between BED and clinical response was registered (p= .04). Independently from the adopted
technique, a pain response was observed (p=
.0005) (Figure 1). Adverse events frequency, including fracture rate, in
both SBRT and conventional treatment group was not significant.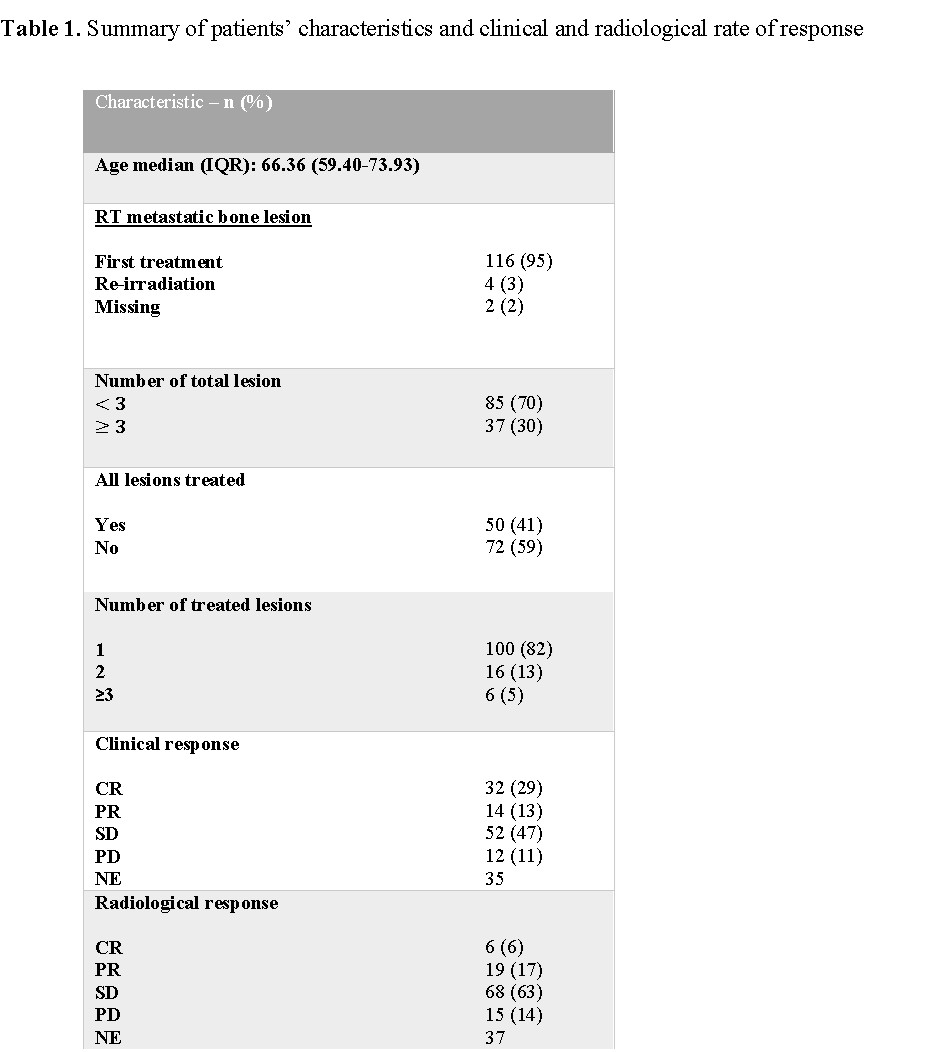
Conclusion
SBRT is superior to conventional RT in terms of pain control
and local disease control. It is important to notice that accurate and uniform
radiological assessment is complicated in retrospective setting. SBRT could represent the standard of care for oligometastatic patients with good performance status and a longer
life expectancy.