Automated and clinical-criteria-driven optimal planning: clinical experience with over 3400 patients
OC-0472
Abstract
Automated and clinical-criteria-driven optimal planning: clinical experience with over 3400 patients
Authors: Linda Hong1, Masoud Zarepisheh1, Ying Zhou1, Qijie Huang1, Gourav Jhanwar1, Jie Yang1, Hai Pham1, Laura Cervino1, Jonathan Yang2, Josh Yamada2, Joseph Deasy1
1Memorial Sloan Kettering Cancer Center, Medical Physics, New York, USA; 2Memorial Sloan Kettering Cancer Center, Radiation Oncology, New York, USA
Show Affiliations
Hide Affiliations
Purpose or Objective
To
present our clinical experience with an automated approach to IMRT treatment
planning using expedited constrained hierarchical optimization (ECHO) to
improve clinical workflow, planning efficiency, and plan quality and
consistency.
Material and Methods
After
contouring, a template using multiple IMRT fields was created and sent to ECHO
through the Eclipse® application program interface (API) plug-in. Institutional clinical
criteria, including maximum and mean doses plus dose volume metrics, were
separated into 2 categories: limits and guidelines. These clinical criteria
were directly employed as template ECHO input parameters to derive appropriate
objective functions and constraints. ECHO optimization strictly enforced limits
as constraints and optimized the guidelines as much as possible using objective
functions. The optimal fluence
map generated by ECHO was imported automatically into Eclipse for leaf
sequencing and final dose calculation. Upon ECHO completion, the planner
received an email indicating the plan was ready for review. The email also
includes a plan quality summary report. The plan was accepted by the planner if
all clinical criteria were met, otherwise a limited number of parameters could be
adjusted prior to another run with ECHO.
Results
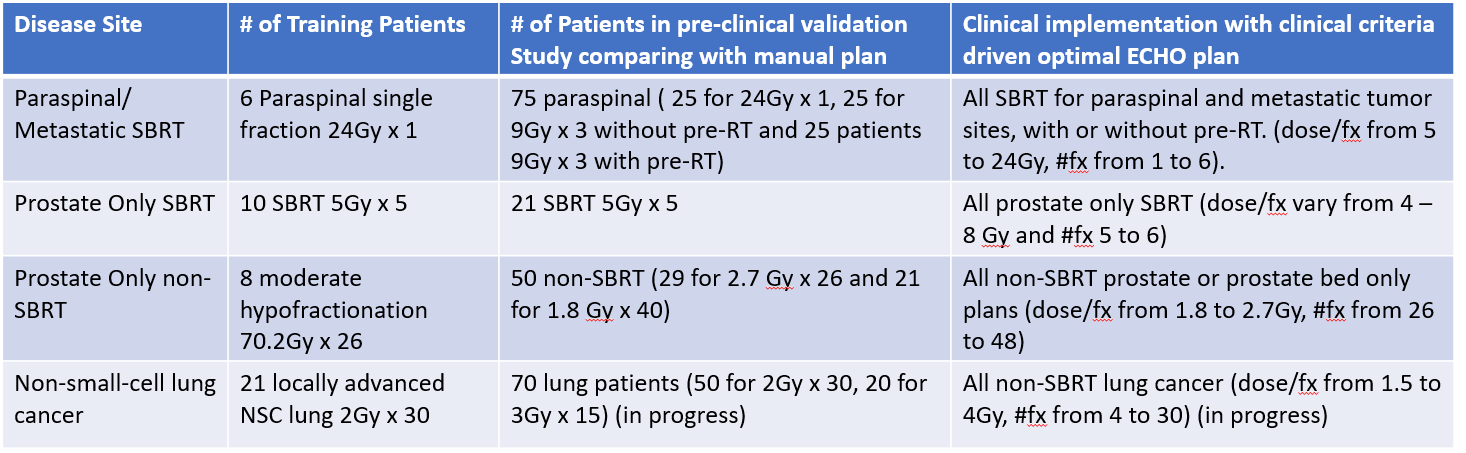
We
have established a process to develop and implement ECHO to the clinic. For
each disease site, a template based on the established clinical criteria (limit
and guidelines) was created and ECHO only required limited representative
training patient data to fine tune few optimization parameters (e.g., dose
fall-off criteria, slip factors). After training, the same parameters were then
used to validation study of slightly more plans with a few prescription schemes
and corresponding clinical criteria and compared with manual plans. Those
parameter templates were then clinically implemented to plan that disease site
with widely different prescription scheme and can easily adapt to changing
clinical practice. Table 1 illustrates details of the process.
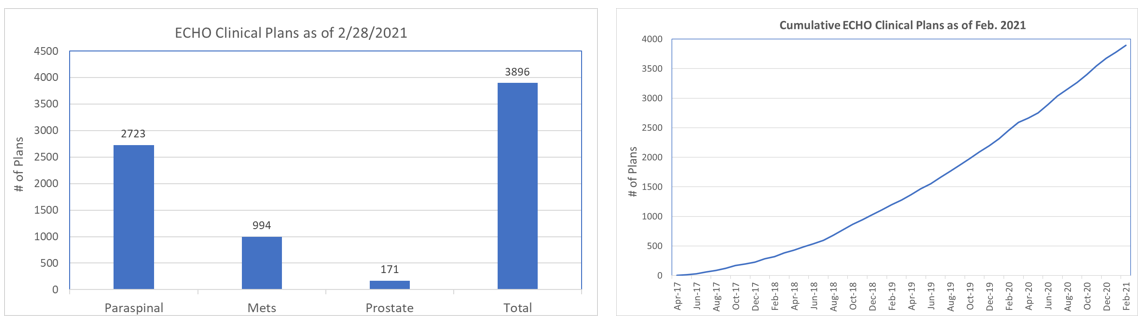
From
4/2017 to 2/2021, 3401 patients underwent radiotherapy using 3896 ECHO produced
plans. Figure below shows treated ECHO plans for different disease sites. PTV sizes varied greatly with median 77 cc
(range 1.5 - 988). The median time to produce one ECHO plan was 29
minutes (range 7 - 168) mainly depending on the PTV size. For prostate plans,
all plans were clinically accepted after single run. For paraspinal/metastatic
tumor SBRT plans, 76% of ECHO plans required only one run.
Conclusion
An automated and
clinical-criteria-driven optimal planning has been established in our institution. ECHO now produces
a majority of SBRT plans for paraspinal and other metastatic tumors in our
clinic. We are rapidly expanding ECHO for prostate, non-small-cell lung cancer
and other disease sites. ECHO improved consistency of plan quality for
treatment planning and enabled expedited treatment including same day SBRT
treatment in our clinic.