Reading Between the Voxels: Radiomic Predictors of Progression-Free Survival in Cervical Cancer
OC-0012
Abstract
Reading Between the Voxels: Radiomic Predictors of Progression-Free Survival in Cervical Cancer
Authors: Ross Zeitlin1, Hina Saeed2, Diane Schott3, Ying Zhang2, Phillip Prior2, Jason Rownd2, Allen Li2, Beth Erickson2, Manpreet Bedi2
1John H. Stroger, Jr. Hospital of Cook County, Radiation Oncology, Chicago, USA; 2Medical College of Wisconsin, Radiation Oncology, Milwaukee, USA; 3University of Nebraska Medical Center, Radiation Oncology, Omaha, USA
Show Affiliations
Hide Affiliations
Purpose or Objective
We recently reported on a single axial T2 SPACE MR-based radiomic predictor for progression-free survival (PFS) in cervical cancer patients. This study aims to identify additional predictors for PFS in patients treated with definitive chemoradiation undergoing serial MR-based planning for every brachytherapy fraction.
Material and Methods
In this retrospective review, 47 patients underwent definitive chemoradiation for stages IB-IV cervical cancer between 2012 and 2018, consisting of intracavitary brachytherapy following external beam radiation. Clinical factors with potential predictive power were analyzed. Sequential MRI scans were acquired on the same 3T scanner with acquisition of T2 SPACE sequences for every fraction (4-5) for each patient during their brachytherapy course. Radiomics feature extraction was performed with an in-house developed software to calculate histogram and Grey Level Co-occurrence Matrix texture features. The HR-CTV was contoured/segmented, the applicator was removed from the HR-CTV contour, and features relating to shape, image intensity, and texture were extracted from the T2 MR sequences from the first and last brachytherapy fractions. The difference between these fractions was calculated for each feature (“delta fraction”). Univariate Cox proportional hazards analysis (UVA) was performed on radiomics features and PFS. The receiver operating characteristic (ROC) analysis was performed to evaluate the performance of prediction model and radiomics nomogram. Kaplan-Meier (KM) survival curves were generated for each selected feature for correlation with PFS at 2 years (PFS2Y).
Results
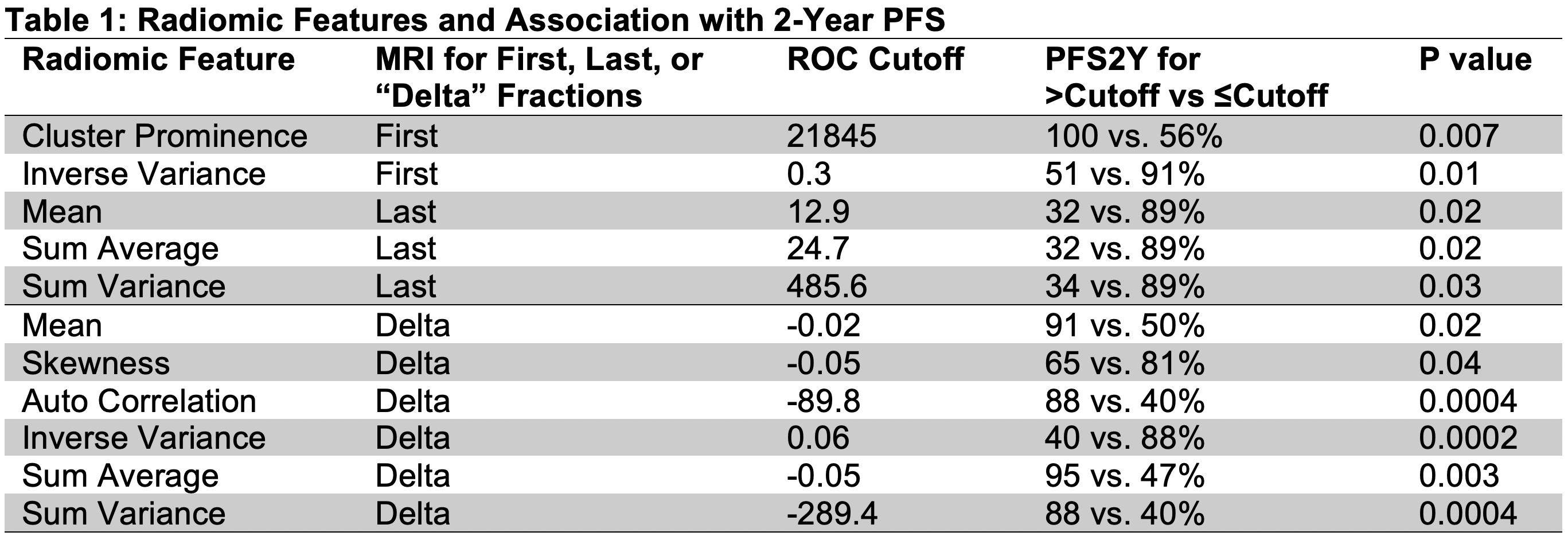
Median patient age is 52 years (26-85). Progression occurred in 17% of patients (8/47), including 4% (2/47) with locoregional relapse, and 13% (6/47) with distant metastasis. PFS2Y was 77%. On UVA, 11 distinct features extracted from the first, last, or delta fraction T2 MR sequences demonstrated a statistically significant correlation with PFS (p<0.05, Table 1). Using the reported cutoff values per ROC analysis in Table 1, the calculated KM curves for each feature showed a statistically significant difference in PFS2Y. Improved PFS was associated with increased first fraction cluster prominence as well as decreased first or last fraction inverse variance, mean, sum average, and sum variance. Improved PFS correlated with increased delta mean, auto correlation, sum average, and sum variance as well as decreased delta skewness and inverse variance.
Conclusion
T2 SPACE MR-based radiomic changes in homogeneity and texture may correlate with improved PFS in this series. These signatures may serve as a prognostic tool in predicting outcomes for patients with cervical cancer. Further research is needed for large scale validation, which may justify more aggressive and personalized treatment in patients identified with a high probability of recurrence.