The impact of weight loss in head and neck cancer patients treated with chemo-radiotherapy
PO-1232
Abstract
The impact of weight loss in head and neck cancer patients treated with chemo-radiotherapy
Authors: chiara lucrezia deantoni1, Laura Giannini1, Martina Midulla1, Anna Chiara1, Andrei Fodor1, Flavia Zerbetto1, Aurora Mirabile2, Sara Cardellini3, Italo Dell'Oca1, Nadia Gisella Di Muzio4
1IRCCS San Raffaele Scientific Institute, Radiation Oncology, Milano, Italy; 2IRCCS San Raffaele Scientific Institute, Unit of Oncology, Medical Oncology Department, Milano, Italy; 3IRCCS San Raffaele Scientific Institute, Nutritional Biology, Milano, Italy; 4Vita-Salute San Raffaele University, Medicine and Surgery, Milano, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
The weight loss is one of the most common consequences in head and neck cancer treatments and plays an important role on worsening short-term quality of life and patient compliance. Its impact on long-term survival is already uncertain.
Material and Methods
In order to standardize the study population, we considered only one-hundred head and neck cancer patients, with locally advanced (stage III-IVA/B) nasopharyngeal or oropharyngeal disease treated in our center with radical intent from 2005 and 2021 with the following schedule:
-Helical TomoTherapy (HT), delivered with a Simultaneous Integrated Boost (SIB) technique: 54 Gy (1.8 Gy/day) to the clinically negative neck region and 66 Gy (2.2 Gy/day) or 69 Gy (2.3 Gy/day) to the tumor and positive nodal regions based on 18FDG CT/PET imaging.
-concomitant platinum-based CT (at least 200 mg/m2).
This population was divided in two subgroups, based on the weight difference between the beginning and the end of radiotherapy: less or equal to 5% (subgroup 1=33 pts) versus more than 5% (subgroup 2=67 pts).
Results
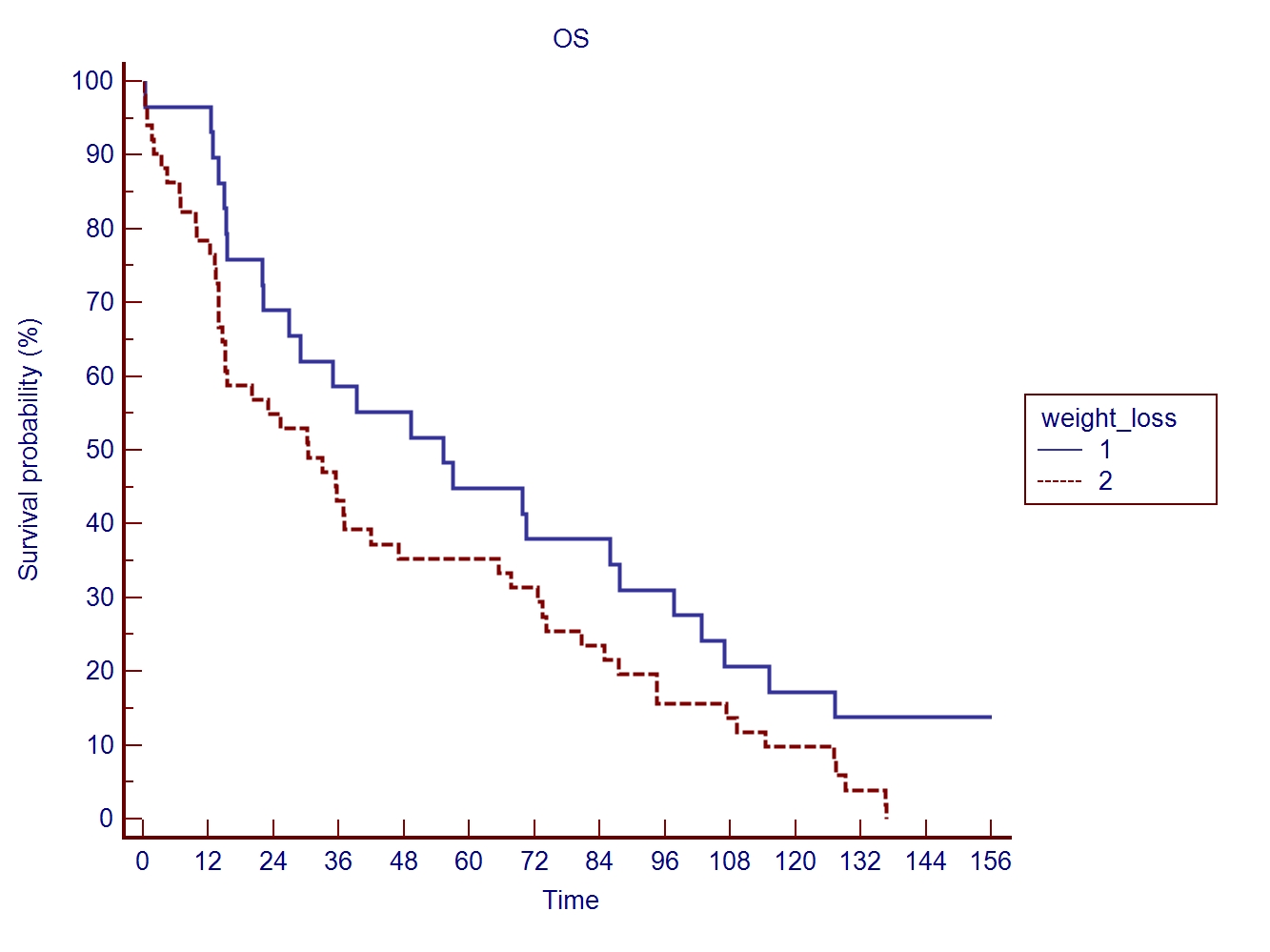
All patients concluded the treatment, without significant interruption. The median weight loss during CT-RT was 7% (range 0-23%). The median overall survival was 52 months (range 3-209). Using Kaplan Meier method the OS was significantly higher in the subgroup with the lower weight loss (fig 1, p-value 0.04)
Conclusion
This analysis is a part of a study in progress in our center, aimed to exploring the role of early nutritional support in improving clinical outcomes in head and neck patients. This study, despite the limitations of a retrospective analysis on a small population, seems to demonstrate that weight loss should not be considered a simple side effect of our treatment but as a factor capable of influencing the prognosis. All interventions aimed at improving nutritional status can have an impact not only on the quality of life but probably also on long-term survival.