Adjuvant Radiotherapy in Node-negative Parotid Gland Malignancies: A Multi-institutional Analysis
JUNG BIN PARK,
Korea Republic of
PO-1211
Abstract
Adjuvant Radiotherapy in Node-negative Parotid Gland Malignancies: A Multi-institutional Analysis
Authors: JUNG BIN PARK1, Hong-Gyun Wu1, Jin Ho Kim1, Joo Ho Lee1, Soon-Hyun Ahn2, Eun-Jae Chung2, Keun-Yong Eom3, Woo-Jin Jeong4, Tack-Kyun Kwon5, Suzy Kim6, Chan Woo Wee6
1Seoul National University Hospital, Radiation Oncology, Seoul, Korea Republic of; 2Seoul National University Hospital, Otorhinolaryngology-Head and Neck Surgery, Seoul, Korea Republic of; 3Seoul National University Bundang Hospital, Radiation Oncology, Seongnam, Korea Republic of; 4Seoul National University Bundang Hospital, Otorhinolaryngology-Head and Neck Surgery , Seongnam, Korea Republic of; 5SMG-SNU Boramae Medical Center, Otorhinolaryngology-Head and Neck Surgery, Seoul, Korea Republic of; 6SMG-SNU Boramae Medical Center, Radiation Oncology, Seoul, Korea Republic of
Show Affiliations
Hide Affiliations
Purpose or Objective
To determine the role of adjuvant radiotherapy (ART) in parotid gland cancer without nodal metastasis, we evaluated the survival outcomes, prognostic factors, and dose-response relationships in patients with node-negative salivary gland malignancies of the parotid gland patients who underwent curative parotidectomy.
Material and Methods
Patients who underwent curative surgery and were pathologically diagnosed with parotid gland cancer without regional or distant metastases between 2004 and 2019 were reviewed. Histological type and grade were reclassified according to the 2022 World Health Organization classification. The benefit of ART in terms of locoregional control (LRC) and progression-free survival (PFS) were evaluated.
Results
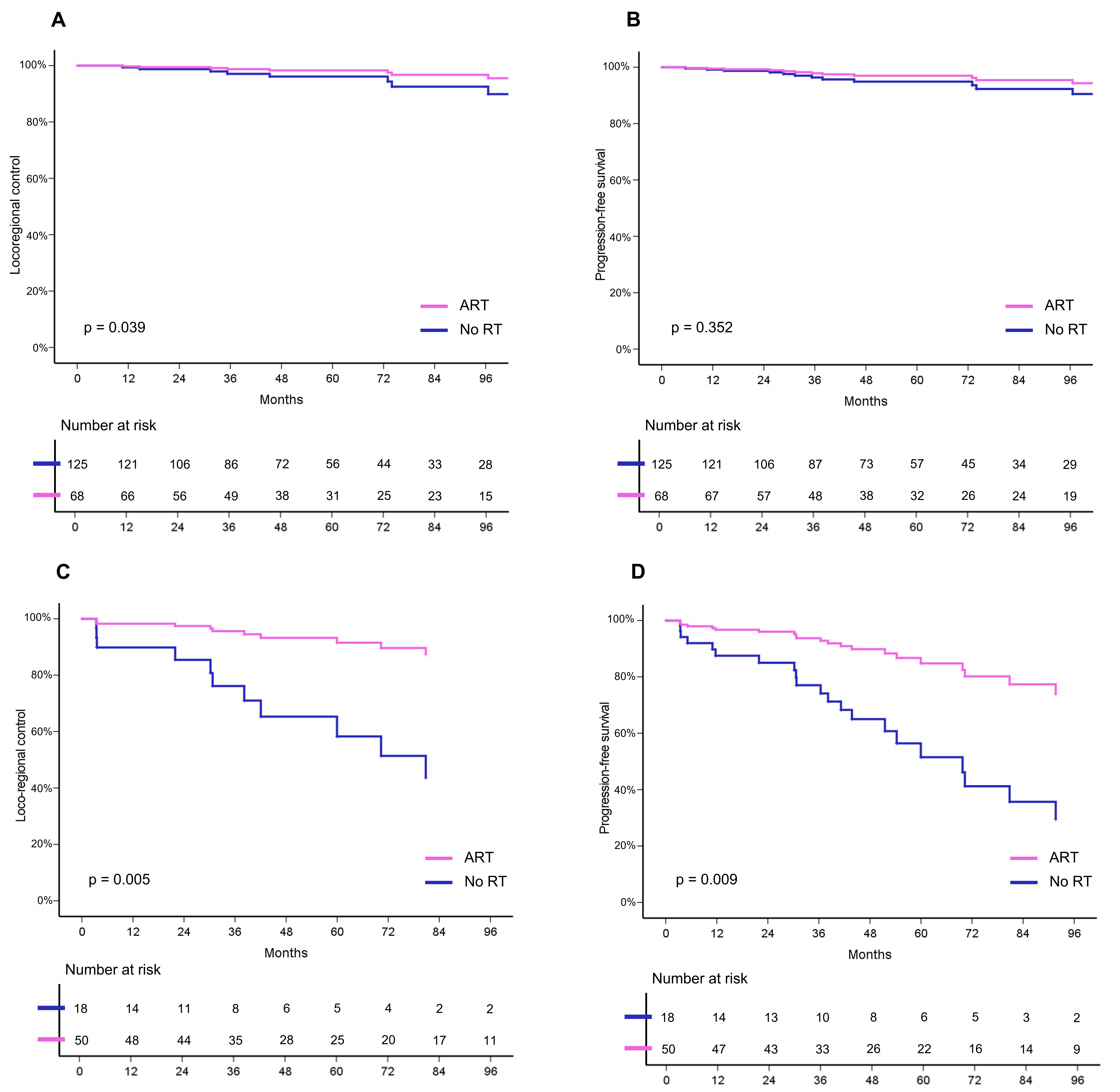
In total, 261 patients were included in the analysis. Among those patients, 45.2% received ART. The median follow-up period was 66.8 months. Multivariate analysis revealed that histological grade and ART were independent prognostic factors for LRC and PFS (all p < .05) (Figure 1). For patients with high-grade histology, ART was associated with a significant improvement in 5-year LRC (adjusted hazard ratio [HR], 0.17; 95% confidence interval [CI], 0.05–0.58; p = .005) and PFS (HR, 0.25; 95% CI, 0.09–0.71; p = .009) in multivariate analysis (Figure 2). Among patients who complete ART and had a high-grade histology, higher biologic effective dose (≥77 Gy10) significantly increased PFS (HR, 0.10 per 1-Gy increase; 95% CI, 0.02-0.58; p = .010). ART significantly improved LRC (HR, 0.18; 95% CI, 0.04–0.92; p = .039) in patients with low-to-intermediate histological grade as well per multivariate analysis. Subgroup analyses revealed patients with T3–4 stage and close/positive resection margins (< 1 mm) would benefit from ART.
Figure 1. [A] Locoregional control and [B] progression-free survival in all patients
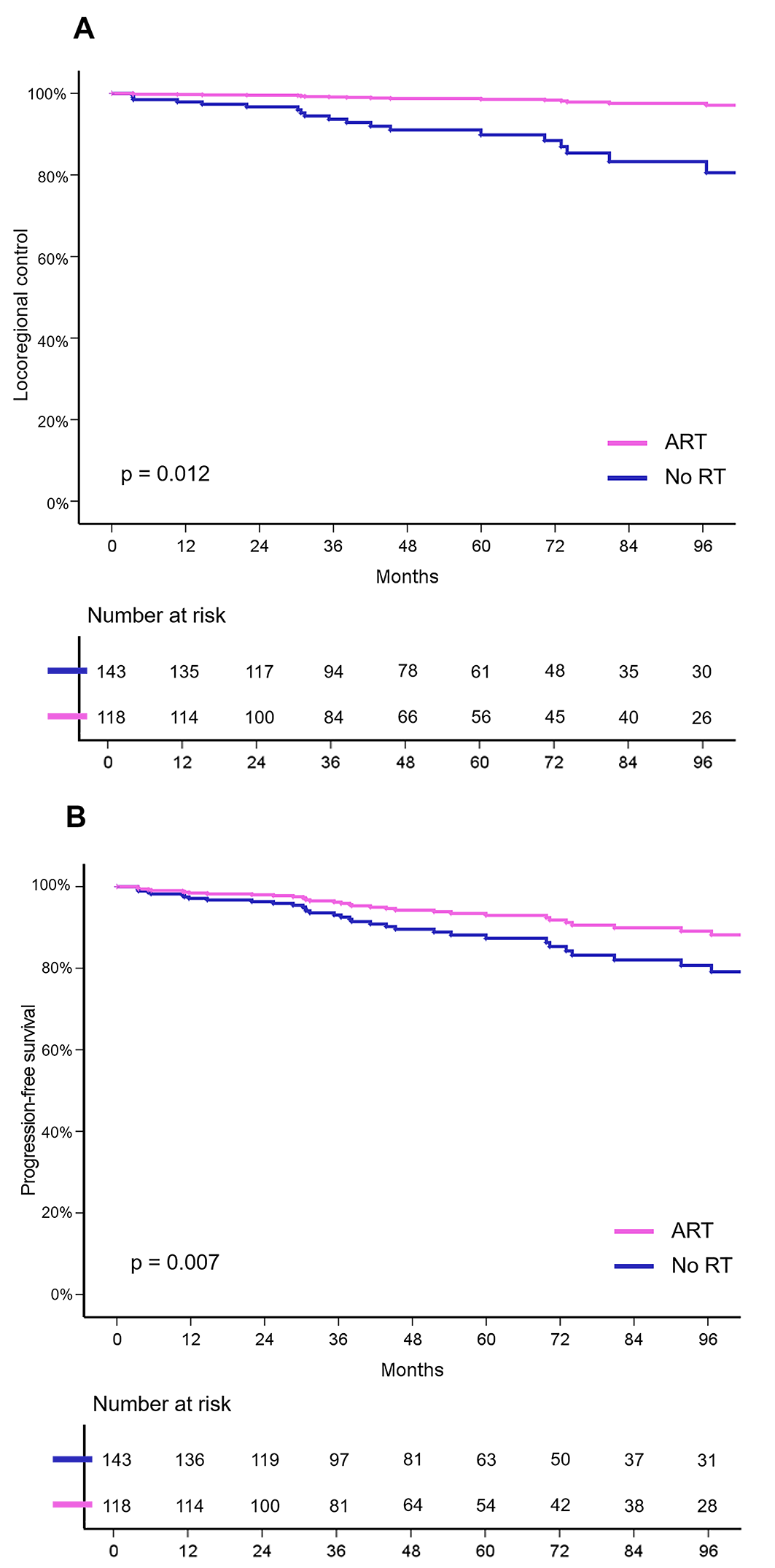
Figure 2. [A] Locoregional control and [B] progression-free survival in patients with low-to-intermediate-grade histology
[C] Locoregional control and [D] progression-free survival in patients with high-grade histology
Conclusion
ART should be strongly recommended for patients with node-negative parotid gland cancer with high-grade histology in terms of disease control and survival. In patients with low-to-intermediate-grade disease, those with adverse prognostic features benefit with ART.