Intensity-modulated radiotherapy for inoperable/unresectable recurrent differentiated thyroid cancer
Jia-Shing Wu,
Taiwan, Province of China
PO-1207
Abstract
Intensity-modulated radiotherapy for inoperable/unresectable recurrent differentiated thyroid cancer
Authors: Jia-Shing Wu1, Yu-Chen Tsai1
1Koo Foundation Sun Yat-Sen Cancer Center, Radiation Oncology, Taipei, Taiwan
Show Affiliations
Hide Affiliations
Purpose or Objective
For differentiated thyroid cancers that recurred in the thyroid bed and/or regional nodal regions, first-line treatments include surgery, percutaneous ethanol injection, and radioactive iodine. However, for inoperable/unresectable lesions, there are few treatment options. Both tyrosine kinase inhibitors and external beam radiotherapy are listed in the guidelines as appropriate, but data supporting their respective efficacies are scarce. We summarize our institutional experience to try to fill the knowledge gap.
Material and Methods
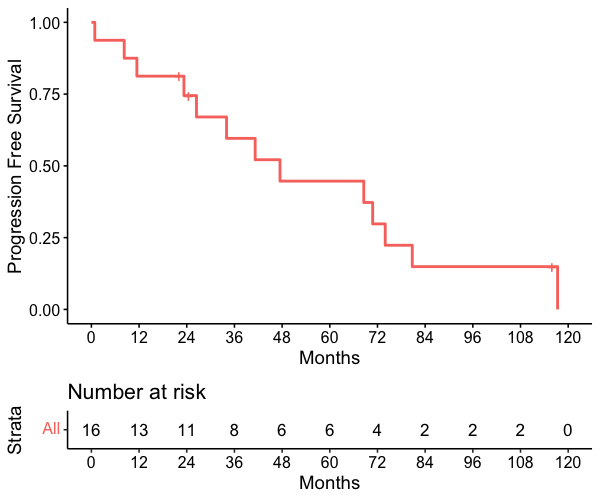
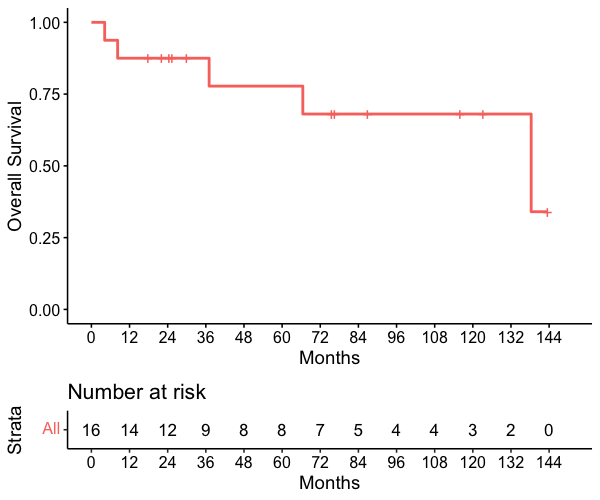
We retrospectively reviewed the medical records of differentiated thyroid cancer patients from 2006-2021 who underwent total thyroidectomy with or without radioactive iodine therapy with inoperable/unresectable recurrence in the thyroid bed and/or regional nodal regions and received intensity-modulated radiation therapy. The primary endpoint was progression-free survival. Secondary endpoints include overall survival and radiation toxicities.
Results
Sixteen patients were identified (male 5, female 11), and the median age was 65 (42-90). All patients had papillary carcinoma and were regarded as iodine-refractory by the referring endocrinologist after having received salvage I-131 therapy with a median cumulative dose of 395 mCi (150-1050). Seven patients (43.7%) had stable lung metastasis before radiation treatment. The patients received intensity-modulated radiotherapy with a median dose of 6700 cGy (6000-7000) in conventional fractionation to the gross tumors with or without elective nodal regions. Ten patients (62.5%) had a more than 50% decrease in tumor markers (thyroglobulin or anti-thyroglobulin) after radiotherapy. Twelve patients (75%) had disease progression that required salvage therapy after radiotherapy (2 local progression, 9 distant progression, 1 both local and distant progression). Five patients received salvage tyrosine kinase inhibitor treatment. The median progression-free survival was 37.6 months (1-117.3), and the median overall survival was 51.8 months (4.2-143.6). The acute radiation toxicities were manageable and no patient had tube dependence or died of late radiation toxicities such as aspiration pneumonia.
Conclusion
Intensity-modulated radiation therapy may provide good local and overall disease control without severe toxicity for differentiated thyroid cancer patients with inoperable/unresectable locoregional recurrence. Radiotherapy may be offered to patients who would like to defer oral tyrosine kinase inhibitors to avoid systemic toxicities. Our data may serve as a reference for discussion with patients for shared decision-making.