Clinical outcomes after re-irradiation with dose painting of head and neck cancer
PO-1181
Abstract
Clinical outcomes after re-irradiation with dose painting of head and neck cancer
Authors: Einar Dale1, Morten Egeberg Evensen2, Cecilie Delphin Amdal1, Torbjørn Furre3, Jon Magne Moan1, Ayca Muftuler Løndalen4, Liv Cathrine Heggebø1, Eirik Malinen5
1Oslo University Hospital, Department of Oncology, Oslo, Norway; 2Drammen Hospital, Vestre Viken Hospital Trust, Section of Oncology, Drammen, Norway; 3Oslo University Hospital, Department of Medical Physics, Oslo, Norway; 4Oslo University Hospital, Department of Radiology and Nuclear Medicine, Oslo, Norway; 5University of Oslo, Department of Physics, Oslo, Norway
Show Affiliations
Hide Affiliations
Purpose or Objective
Dose painting have the potential to increase loco-regional control in head and neck cancer (HNC) without added morbidity. Recurrent or second primary disease overlapping with previously treated volumes is a clinical problem due to the limited tolerance of the irradiated tissues. Patients with recurrent disease could benefit from dose painting, as the focus is on delivering maximal dose to areas of high tumor burden while not exceeding dose constraints to organs at risk (OAR). In this study, we compare the clinical outcome of one group receiving our standard re-irradiation regimen with a group receiving FDG-PET/CT guided dose painting by contours (DPBC).
Material and Methods
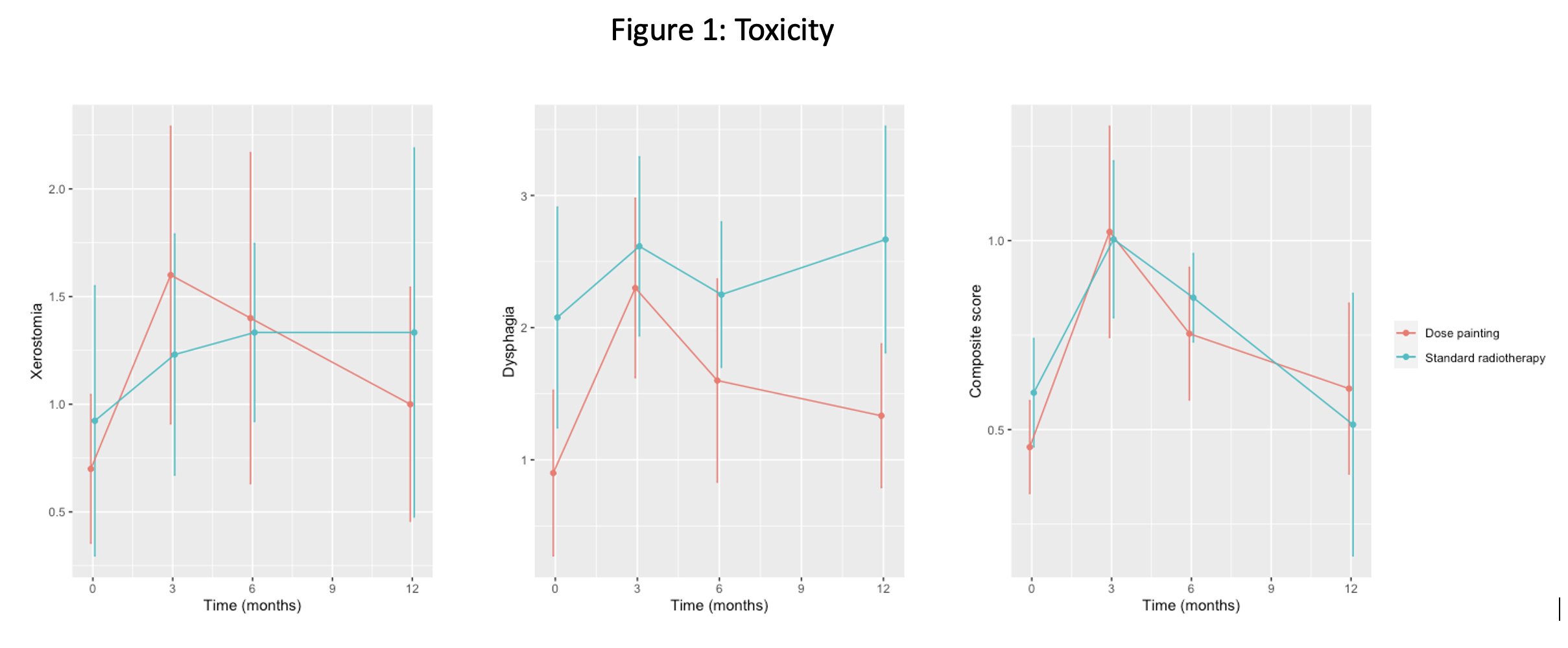
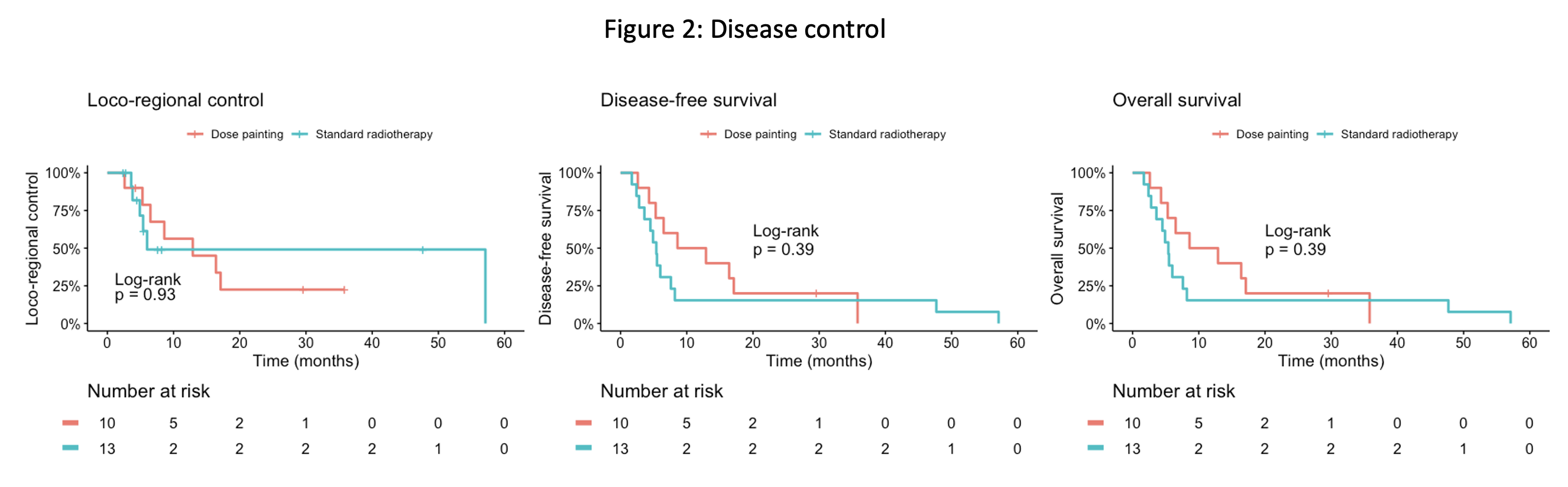
Our conventional re-irradiation regimen is hyperfractionated radiotherapy 1.5 Gy twice daily over four weeks, giving a total dose of 60 Gy. For three-level DPBC, we defined two prescription volumes in addition to CTV; PV33 and PV66, corresponding to 33% and 66% of the highest FDG uptake in the tumor, respectively. The CTV prescription dose was 60 Gy, PV33; 65 Gy and PV66; 70 Gy and Dmax 75 Gy. Thirteen patients who had followed our conventional re-irradiation protocol were compared with ten patients who had received dose painting (ClinicalTrials.gov Identifier: NCT02921581). Toxicity (CTCAE version 3.0) was scored for thirteen separate parameters including xerostomia and dysphagia at baseline, 3, 6 and 12 months after treatment. Furthermore, a composite score; the mean value of all thirteen parameters was calculated. The mean toxicity scores of all patients in each group (with 95% confidence intervals) at each time point were calculated. Disease-related endpoints were loco-regional control, disease-free survival and overall survival. The Kaplan–Meier method was used to analyze survival and the log-rank test was applied to compare survival curves.
Results
Dose painting resulted in an increase in D2cc (highest dose to 2cc volume) of typically 10 Gy compared to conventional therapy when treatment plans were summed with the primary treatment series. The mean toxicity score was maximal 3 months after radiotherapy, with some variation between endpoints (Figure 1). Comparing each time point, no significant difference in toxicity was found between the two groups except for dysphagia at 12 months where the standard group had worse dysphagia scores (p = 0.01). One-year disease free survival was 50% and 15% for dose painting and conventional radiotherapy, respectively, although log-rank tests for the various disease endpoints did not reveal any significant differences (Figure 2).
Conclusion
Three-level dose painting of recurrent head and neck cancer to a maximum dose of 75 Gy did not increase toxicity compared with conventional re-irradiation. We did not find any evidence of improved disease control with dose painting. Still, the dose painted increase in dose of typically 10 Gy is expected to give a benefit in selected patients, and a challenge in future studies is to identify these patients.