Optimising cervix brachytherapy planning using OAR dose estimates from external beam RT daily CBCTs
Elisha Tassano-Smith,
United Kingdom
PD-0499
Abstract
Optimising cervix brachytherapy planning using OAR dose estimates from external beam RT daily CBCTs
Authors: Elisha Tassano-Smith1, Antony L Palmer1, Wojciech Polak1
1Portsmouth Hospitals University Hospitals NHS Trust, Medical Physics, Portsmouth, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Cervical cancer is prescribed EBRT and brachytherapy (BT) to achieve a D90% for the HRCTV above 85 Gy [1]. Current BT practice assumes OARs (bladder, rectum, sigmoid, bowel) receive a dose equal to the EBRT target prescription dose. This assumption lacks supporting data [1-6].
The actual delivered OAR dose may differ from the assumed dose and lead to sub-optimal BT plan optimisation for OAR sparing and HRCTV dose escalation. No previous studies have been found investigating this issue.
We propose a methodology for optimising BT planning by considering an estimate of the actual EBRT OAR dose. This is derived by recalculating the treatment plan on daily CBCT images, with deformed OAR contours. The dose to the highest irradiated volume (D2cc) on each daily CBCT is accumulated to determine a maximum estimate of delivered EBRT OAR doses.
Material and Methods
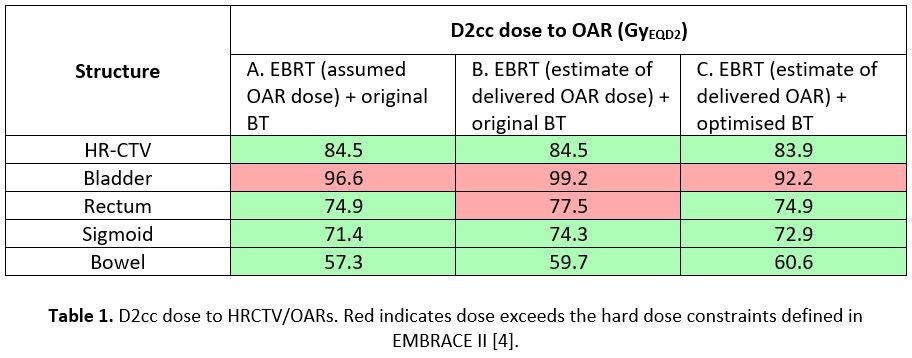
Three methods were used for calculation of total OAR dose:
A) EBRT (assumed OAR dose = target prescription) + original BT
B) EBRT (estimate of delivered OAR dose from daily CBCT) + original BT
C) EBRT (estimate of delivered OAR dose from daily CBCT) + optimised BT
The method was used for one patient as a proof of concept. The contours were propagated onto the CBCT data set with a rigid and deformable registration, manually edited and checked by qualified staff.
The planned EBRT treatment was recalculated in Pinnacle via a validated CBCT to ED curve [7]. The D2cc was reported for each OAR (excluding high dose regions near involved nodes not relevant to BT). This was repeated on all CBCTs with D2cc doses summed giving a maximum estimate of the accumulated EBRT OAR dose. This was converted to EQD2 and used to replan the original BT plan in BrachyVision.
Results
The process was used successfully to give an estimate of the maximum OAR EBRT delivered dose. The results in Table 1 show a difference in the combined EBRT+BT dose calculated by method A and B. When the EBRT dose was changed from the original assumption to the best-estimate of delivered dose, the rectum dose exceeded the mandatory constraint. The rectum dose was brought back into tolerance by replanning the BT with the estimate of delivered EBRT OAR dose (method C, Table 1) at the expense of reducing the HRCTV dose by 0.6 Gy (EQD2). A clinician was consulted and favoured the rectum sparing plan.
In all cases the bladder dose exceeded mandatory tolerance as per a clinical decision to accept higher dose due to bladder involvement.
Conclusion
We proposed a novel method using an estimate of delivered EBRT OAR doses when planning BT. In the case presented, a differently optimised BT plan would have been used clinically by the CCO.
Further work will determine the magnitude of changes in OAR doses that will lead to clinically meaningful differences in the optimisation of BT planning and determine the related uncertainty and decision criteria.