Failure Mode and Effects Analysis for Improving the quality of treatment Planning In Radiotherapy
Sheng-Fang Huang,
Taiwan, Province of China
PO-2308
Abstract
Failure Mode and Effects Analysis for Improving the quality of treatment Planning In Radiotherapy
Authors: Sheng-Fang Huang1, Chih-Chieh Chang1, Jo-Ting Tsai1, Wei-Kai Chuang1, Chun-Yuan Kuo1, Li-Jhen Chen1, Ming-Hsien Li1
1Shuang Ho Hospital, Taipei Medical University, Radiation Oncology, New Taipei City, Taiwan
Show Affiliations
Hide Affiliations
Purpose or Objective
The purpose of this study is to use the failure mode and effects analysis (FMEA) to identify high-risk failure modes of the treatment planning process and to promote the medical quality and patient safety by improving the planning compliance rate in radiotherapy.
Material and Methods
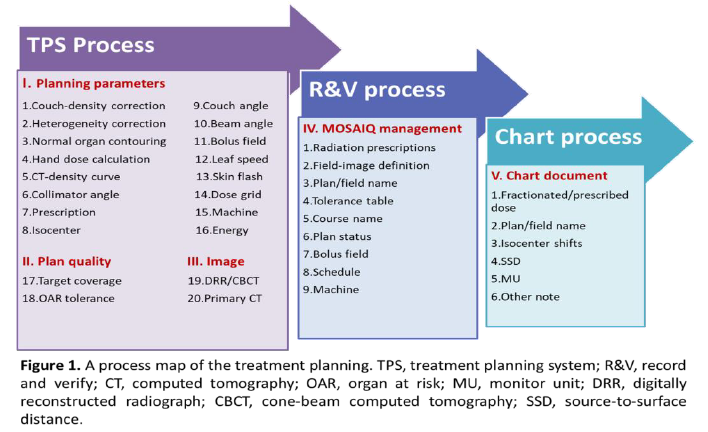
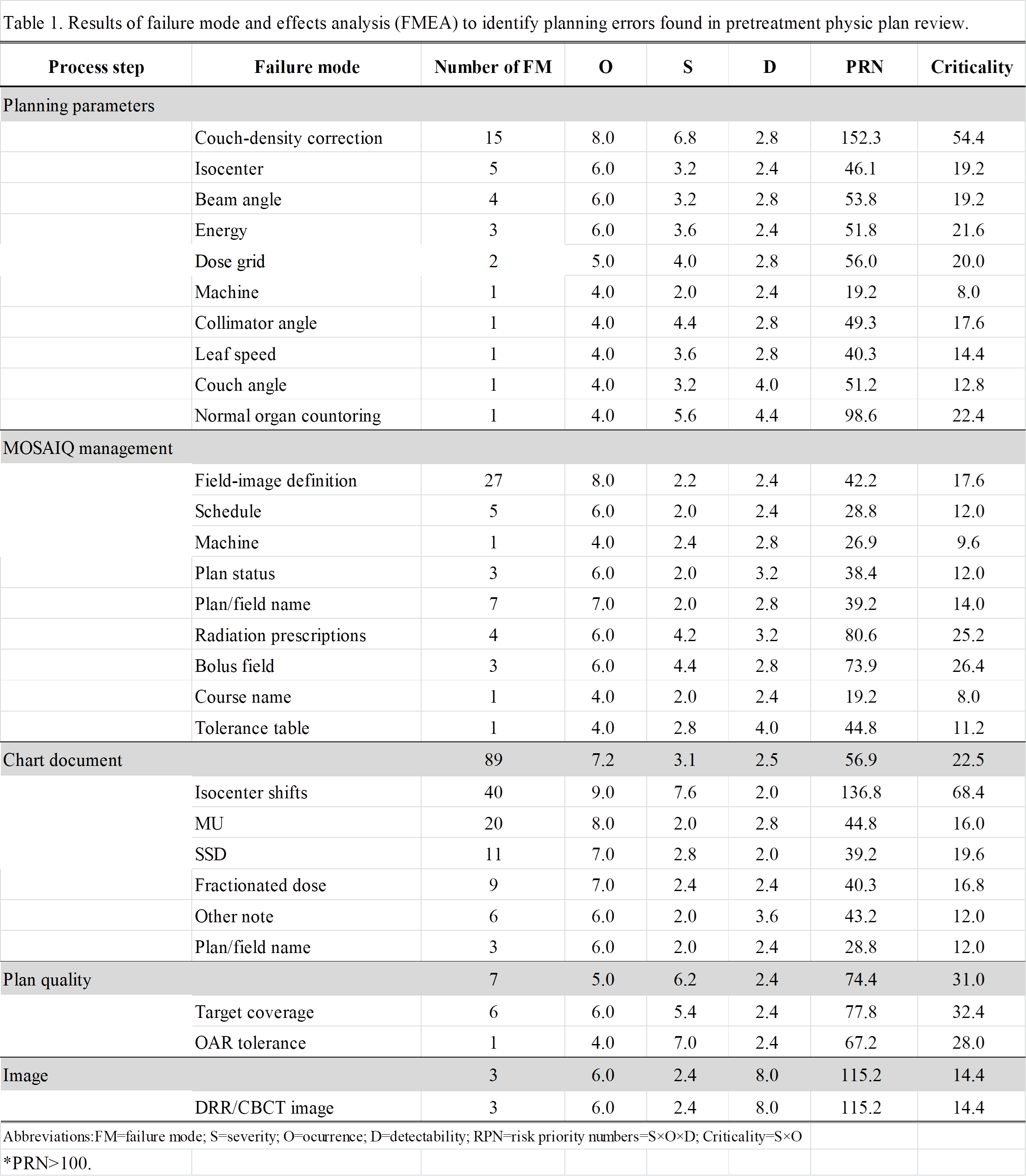
Retrospective analysis was applied to treatment plans in 2020-2022. A process map of the treatment planning including a major process tree and subprocess steps was generated based on the guidelines in TG-100 report. Five major treatment planning process steps were (I) planning parameters, (II) plan quality, (III) image parameters, (IV) MOSAIQ management, and (V) chart documents. Errors detected during or after the PTPCR were identified to failure modes (FMs) in each process step. A risk priority number (RPN=O×S×D) was assigned to each FM by the five physicists based on tabulated scoring system (Table 1) for the frequency of occurrence (O), the severity (S), and the detectability (D) of errors, each on a scale of 1 to 10. The planning compliance rate (= the number of plans without errors the total number of plans × 100%) was calculated to evaluate the quality of the treatment planning. FMs with RPN scores >100 were high risk defined in TG-275 report. High RPNs indicate more critical defect in process. Some Interventions given to improve the planning compliance rate were the couch-density replacement script, the plan/verification-image transmission script, beam-renaming script and the integrated radiation oncology information system (IROIS). The target value of the compliance rate is set to 90% to check if the interventions were effective. The PDCA (Plan-Do-Check-Act) method is used to review the improving process of and to evaluate the strategies.
Results
Figure 1 shows the process map of the workflow of treatment planning at our department. Based on the FMEA results, we found ten key high‐risk failure modes (RPN ≧100). Table 1 presents the FMEA results. The compliance rate of treatment planning was 78.ˇ% in 2020 and then was raised to 89.% in 2021 after our interventions . The data analysis of this year is in progress.
Conclusion
The FMEA provided a useful method for evaluating the errors detected in the PTPCR. The FMEA results and the planning compliance rate could help us to improve the quality of treatment planning and to ensure the patient safety during radiation therapy.