Comparison of immobilisation, imaging and set-up errors during head and neck radiotherapy
PO-2273
Abstract
Comparison of immobilisation, imaging and set-up errors during head and neck radiotherapy
Authors: Lisa Hay1, Lynsey Devlin1, Aileen Duffton1
1The Beatson West of Scotland Cancer Centre, Radiotherapy, Glasgow, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Head and neck cancer (HNC) requires robust immobilisation, with thermoplastic masks, to ensure safe delivery of radiotherapy (RT) dose to planning target volumes. RT technique precision has evolved over the past decade optimising dose delivery, however, neck flexion and shoulder position may vary daily requiring repeat imaging on set-up. These variations can change the treatment plan dosimetry due to the steep dose gradients.
This evaluation aimed to compare immobilisation systems, report the set-up errors for each and determine which reduced imaging frequency during treatment.
Material and Methods
This prospective comparison was undertaken between September 2021 and March 2022. All HNC patients and subsites were included. Patients were selected consecutively from the RT patient management system. All patients were positioned with the pro-step knee rest and one of the below systems (a,b,c).
Immobilisation systems;
a) Klarity 2.4mm thick (15% perforation) 5-point head and shoulder mask, foam headrest (HR).
b) Klarity 2.4mm thick (15% perforation) 5-point head and shoulder mask, foam HR plus an additional individualised accu-cushion placed on the HR and moulded to the patients neck.
c) Portrait 3.2mm thick S-Frame mask with reinforced strips at the forehead, chin and shoulders, a plastic silverman HR and accu-cushion under the neck.
The Klarity masks were connected to the IMRT board attached at the end of the treatment bed. The Portrait masks connected to an overlay board placed on top of the treatment bed, secured by a locking bar.
IGRT involved acquisition of daily online 2D-KV orthogonal images, with shifts applied pre-treatment delivery. Patient’s were reset-up and reimaged where gross error was obvious on acquired images to improve neck flexion, rotation and lateral movement.
Data collected included the number of reset-ups, the total 2D-KV images acquired and the mean 2D-KV images over a treatment course. Systematic and random errors were calculated. The Anova one-way and Tukey tests were used to compare mean shifts between the groups using the SSPS system, p≤0.05.
Results
51 patients were included. All received radical RT over 30 fractions, except 1 patient in group (c) who had 20#s.
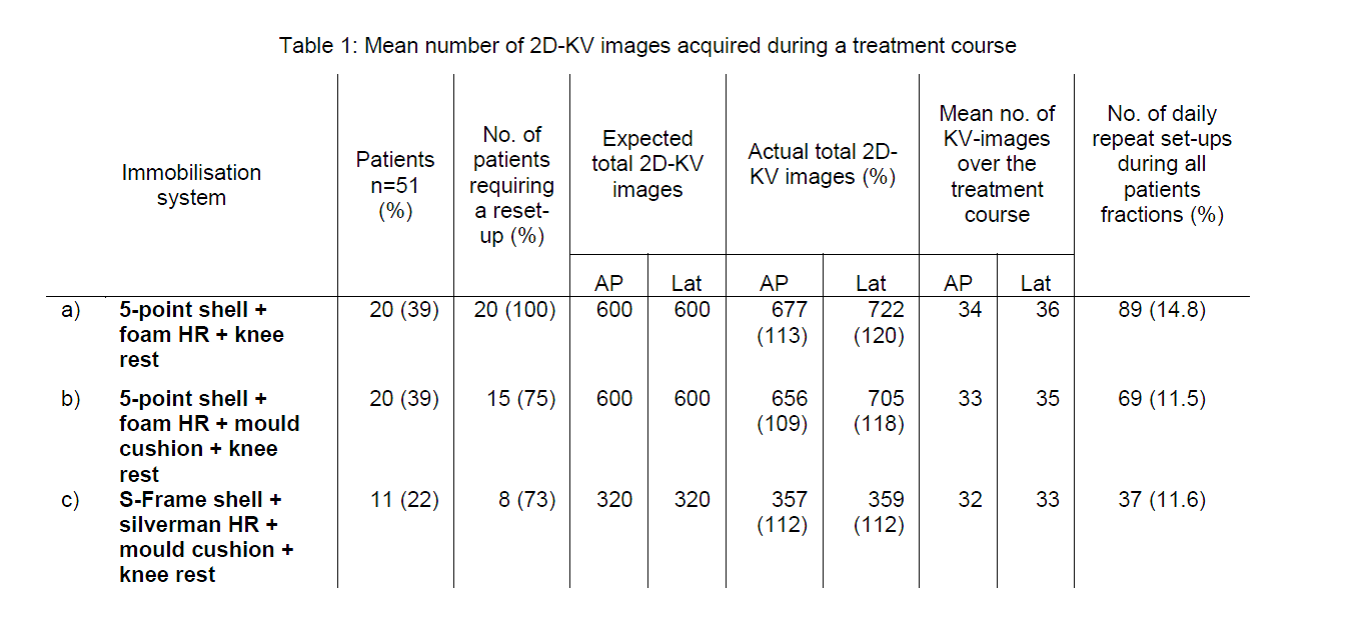
For groups a) and b) 1200 images were expected over a treatment course in each group, however 199 (16.6%) additional images were acquired in group a) and 161 (13.4%) in group b). For group c) there was 76 additional (11.9%) images of an expected 640. Table 1 displays a breakdown for each cohort.
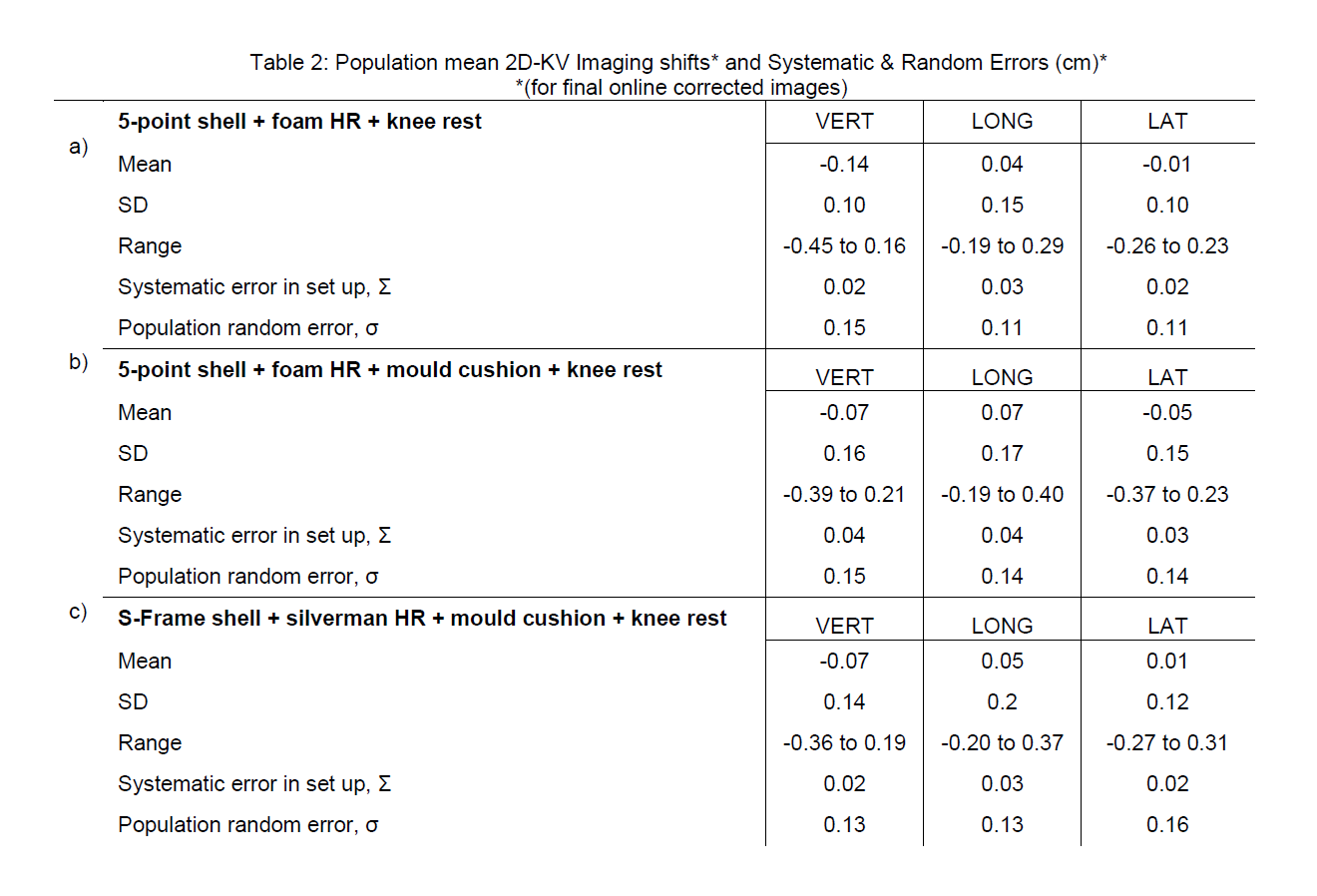
Population mean imaging shifts, SD, range, systematic and random set-up errors are shown in table 2.
The mean shifts between the groups do not differ significantly in any direction, vert F(2, 48)=1.65, p≤0.20, long F(2, 48)=0.19, p≤0.83 and lat F(2, 48)=0.71, p≤0.50.
Conclusion
Image acquisition reduced in the groups with a personalised neck cushion. The portrait system improved neck flexion reducing lateral KV imaging, however further evaluation of system (c) with a larger patient cohort is required.