Does the presence of Magtrace preclude adaptive breast radiotherapy on an MR-Linac?
PO-2267
Abstract
Does the presence of Magtrace preclude adaptive breast radiotherapy on an MR-Linac?
Authors: Lucy Davies1, Lisa McDaid1, Carmel Anandadas2, Philip Fendall Amaro1, Robert Chuter3,4, David Woolf2,4, Cynthia Eccles1,4
1The Christie NHS Foundation Trust, Radiotherapy, Manchester, United Kingdom; 2The Christie NHS Foundation Trust, Clinical Oncology, Manchester, United Kingdom; 3The Christie NHS Foundation Trust, Radiotherapy Physics, Manchester, United Kingdom; 4University of Manchester, Division of Cancer Sciences, Manchester, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
This work reports on a finding that impaired image quality in the preparation work for the clinical implementation of MR-guided adaptive radiotherapy (MRgART) for accelerated partial breast irradiation on an Elekta Unity MR-Linac (MRL) (Elekta AB. Stockholm, Sweden).
Material and Methods
A patient with T2 N0 M0 right breast invasive ductal carcinoma, receiving adjuvant radiotherapy, was recruited to an approved imaging study, PRIMER (Clinicaltrials.gov NCT02973828). The patient underwent two volunteer breast imaging sessions on the MRL, positioned supine, with arms above head on an in-house manufactured thorax board with individualised vacuum-moulded bag (100x70cm 20 litre fill; Klarity Medical Products, Ohio, USA). A combination of T1- and T2-weighted (W) turbo spin echo (TSE) sequences were acquired alongside T1W mDIXON sequence. A T2W TSE sequence was acquired on end-expiration using a navigator pulse. All images were reconstructed in the axial plane (Table 1).
All images were assessed for image quality using visual grading analysis (VGA), and appropriateness for use within the treatment pathway. During the VGA, an artefact in the right breast was noted by the independent observers (2 MRL Radiographers and 1 Oncologist). The patient was rechecked for anything on the skin and medical notes were reviewed for any possible explanation. The findings were discussed with the patient’s Clinical Oncologist and referred to local multi-disciplinary team (MDT) for radiologist review.
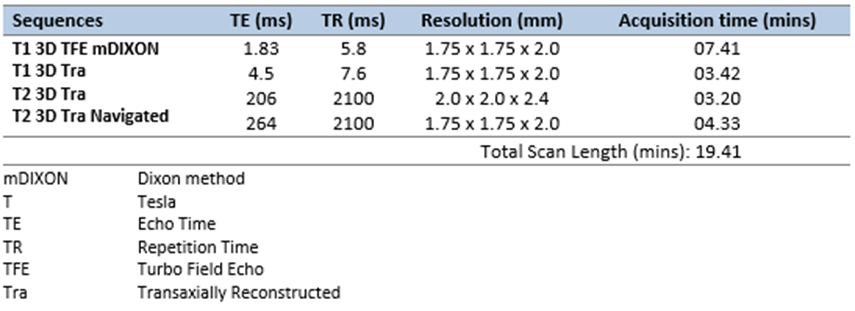
Table 1: MRL Scan Sequence
Results
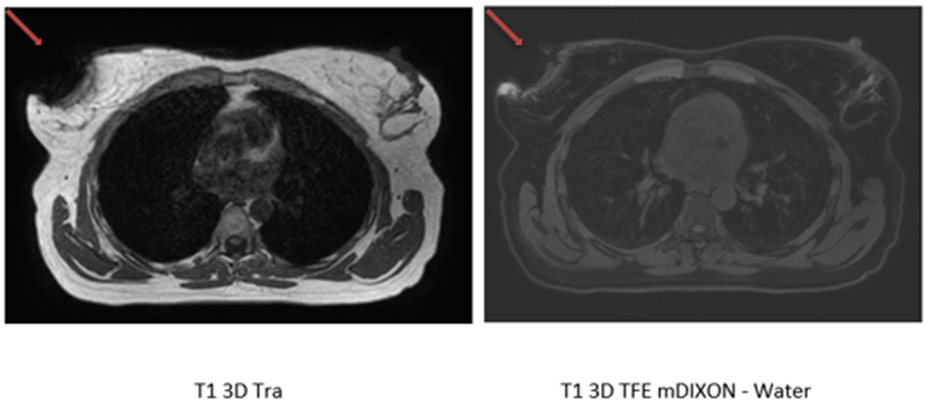
On further investigation, assessment of the patient’s MRL images demonstrated a signal void in the right breast that coincided with the surgical site (Figure 1). This was distal from the tumour bed and deemed unlikely to be related to a Magseed marker or intraoperative clips. The patient reported no history of nipple tattoo or piercing. There was nothing on clothing that this could be attributed to.
This case was referred to local MDT for review of the pathology specimen and x-ray-based imaging. MDT confirmed both the Magseed and radiological markers were present in the pathological sample but suggested a probable cause for the artefact to be Magtrace, which is routinely used. A differential cause of haemosiderin was discounted due to the length of time between surgery and imaging. No further patient follow-up was required.
Figure 1: Axial MR slice across two imaging sequences. The red arrow indicates the signal void in the right breast.
Conclusion
Magtrace, a superparamagnetic iron oxide tracer, is recommended as an option to locate sentinel lymph nodes (SLNs) for breast cancer (NICE, 2022). The use of Magtrace caused significant image artefacts in this patient, potentially making them not suitable for the MRL. Further investigation into the widespread surgical adoption of Magtrace for SLN identification and the potential impact on accuracy of contouring and treatment plans when considering MRgART needs to be considered when setting up the service.