GI factors, prevalence of and potential to affect motion during radiotherapy. A scoping review
Sophie Alexander,
United Kingdom
PO-2262
Abstract
GI factors, prevalence of and potential to affect motion during radiotherapy. A scoping review
Authors: Sophie Alexander1, Helen.A. McNair1, Uwe Oelfke2, Alison.C. Tree3
1The Royal Marsden NHS Foundation Trust/ The Institute of Cancer Research, Radiotherapy, Sutton, United Kingdom; 2The Royal Marsden NHS Foundation Trust/ The Institute of Cancer Research, The Joint Department of Physics, Sutton, United Kingdom; 3The Royal Marsden NHS Foundation Trust/ The Institute of Cancer Research, Uro-oncology, Sutton, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
The probability and magnitude of prostate motion during radiotherapy is associated and increases with rectal distension[1-6]. Rectal filling is the product of digestive events occurring throughout the GI tract and is influenced by intrinsic patient and environmental factors[7]. We hypothesise that these factors, which affect bowel function and rectal filling, consequently impact prostate motion. If true, patient specific measurement of these GI-factors could predict motion uncertainty during radiotherapy, facilitating personalised care by optimising treatment technique e.g., daily adaption or via bespoke patient pre-habilitation and preparation.
A scoping literature review was completed to identify GI-factors most likely to influence prostate motion during radiotherapy and establish reliable, quick methods of quantifying these in a busy clinic.
Material and Methods
Published scoping review methodology[8], literature identification, screening, and eligibility guidance[9] were followed. Two preliminary OVID MEDLINE® searches established common terms relating to lower GI motion and morbidity and identified predominant GI-factors.
For predominant GI-factors a search strategy was created, using terms identified in preliminary searches. Searches were run on four databases: Ovid Medline®, EMBASE, CINAHL and EBSCO discovery. Articles written in English from 2010-present were included. Those pertaining to paediatrics, biological women exclusively, infectious and post-treatment GI morbidity and diet were excluded.
Articles were grouped by causative factor to establish prevalent sub-factors and examine specific GI symptoms, incidence and assessment tools. The prevalence of common sub-factors in a prostate cancer population was estimated.
Results
The preliminary search for GI-factors (May 2021) yielded 489 articles, 87 met the inclusion/exclusion criteria. Four prominent GI-factors presented (Figure 1).
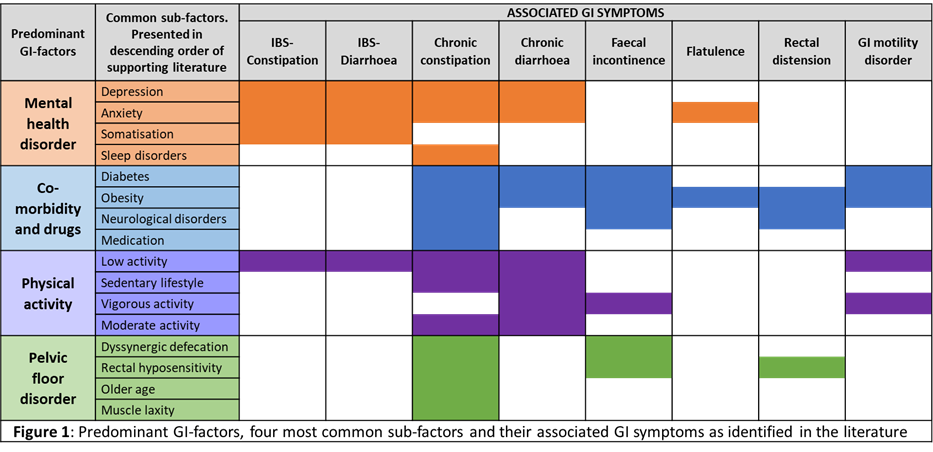
The GI-factor search (Feb. 2022) found 3644 articles; 1646 were removed as duplicates. A further 1249 were excluded after title and abstract screening, 162 remained subsequent to full text review: 42 mental health, 53 co-morbidity and medication, 39 physical activity and 28 pelvic floor disorder. Sixteen common sub-factors were identified, Figure 1 presents these and their associated GI symptoms.
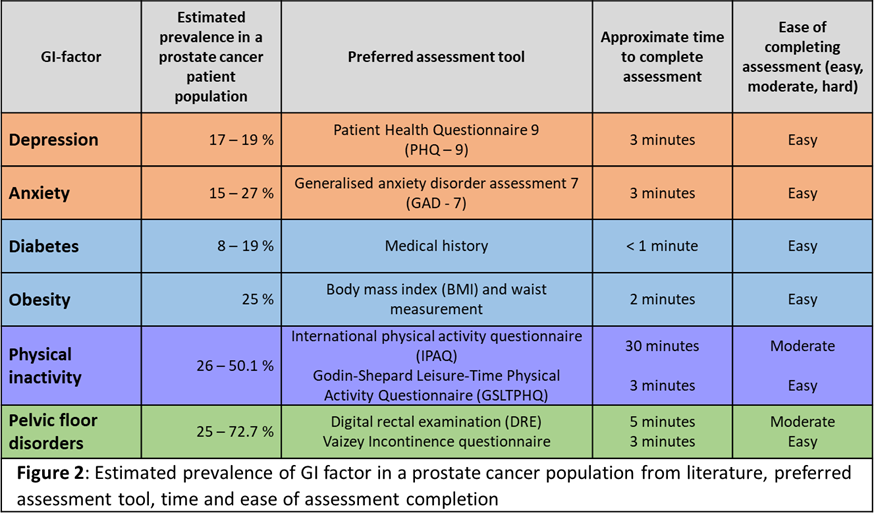
Prevalence of depression, anxiety, diabetes, obesity, low physical activity, and pelvic floor disorder was estimated to be considerable in a prostate cancer population. Reliable assessment tools are available and quick to complete (Figure 2).
Conclusion
Sixteen GI-factors were identified. The most common six factors appear prevalent in a prostate cancer population. Reliable, quick, and easy to use tools are available to quantify these factors.
We are introducing these tools to clinic practice, to establish prevalence of GI-factors in our prostate cancer population, evaluate their effect on inter- and intrafraction prostate motion and guide provision of personalised treatment and care.