On the implementation of a clinical workflow for the Transit-Guided Radiation Therapy technique
Elisabet Escudero ,
Spain
PO-2261
Abstract
On the implementation of a clinical workflow for the Transit-Guided Radiation Therapy technique
Authors: Elisabet Escudero1, Cristina Castro1, Artur Latorre-Musoll1, Sergi Serrano1, Gabriela Oses1, Gabriela Antelo1, Meritxell Mollà1
1Hospital Clínic de Barcelona, Oncologia Radioteràpica (ICMHO), Barcelona, Spain
Show Affiliations
Hide Affiliations
Purpose or Objective
The lack of reproducibility of the patient positioning is one of the major contributors to geometric uncertainties in the radiotherapy chain. Transit-Guided Radiation Therapy (TGRT) is a novel technique that has been proposed to provide reliable on-line corrections to position errors by assessing the transit portal images (TPIs) of the treatment fields (Phys Med Biol 2022 67 155022).
In this work we describe the clinical workflow used to implement the TGRT technique within an ongoing prospective clinical study aimed to validate this technique in a clinical setting.
Material and Methods
Despite the TGRT technique may be broadly applicable to all treatment sites and techniques, only whole-brain and breast treatments have been included for validation purposes in the current clinical study.
The TGRT technique is an in vivo technique that acquires the TPIs of the treatment fields using the Electronic Image Portal Device (EPID) as a passive radiation detector (i.e., the treatment delivery is not perturbed). Thus, some parameters must be defined in Eclipse/Aria/TrueBeam environment, namely:
- The "Integrated Image" image template is scheduled in all treatment fields and fractions.
- The EPID is deployed at (Lat = Lng = 0, Vrt = SDD), i.e., centred with respect the beam axis and at a safe source-to-detector distance (SDD) to minimize the risk of collision (typically, SDD = 150 cm for brain and SDD = 170 cm for breast).
Before the delivery, a dry-run is performed to check the EPID clearance or, eventually, to change the SDD to a safe position.
TPIs are exported and assessed after treatment completion.
Results
The clinical study is still open. Up to now, the TGRT technique could be satisfactorily applied to all enrolled patients (29 patients, 506 field/fraction combinations). Treatment time has not been impaired and EPID collisions have not been an issue.
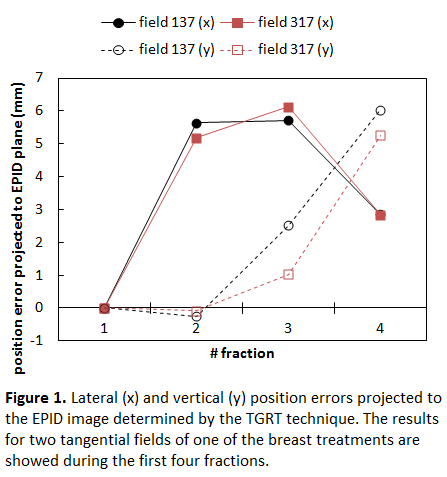
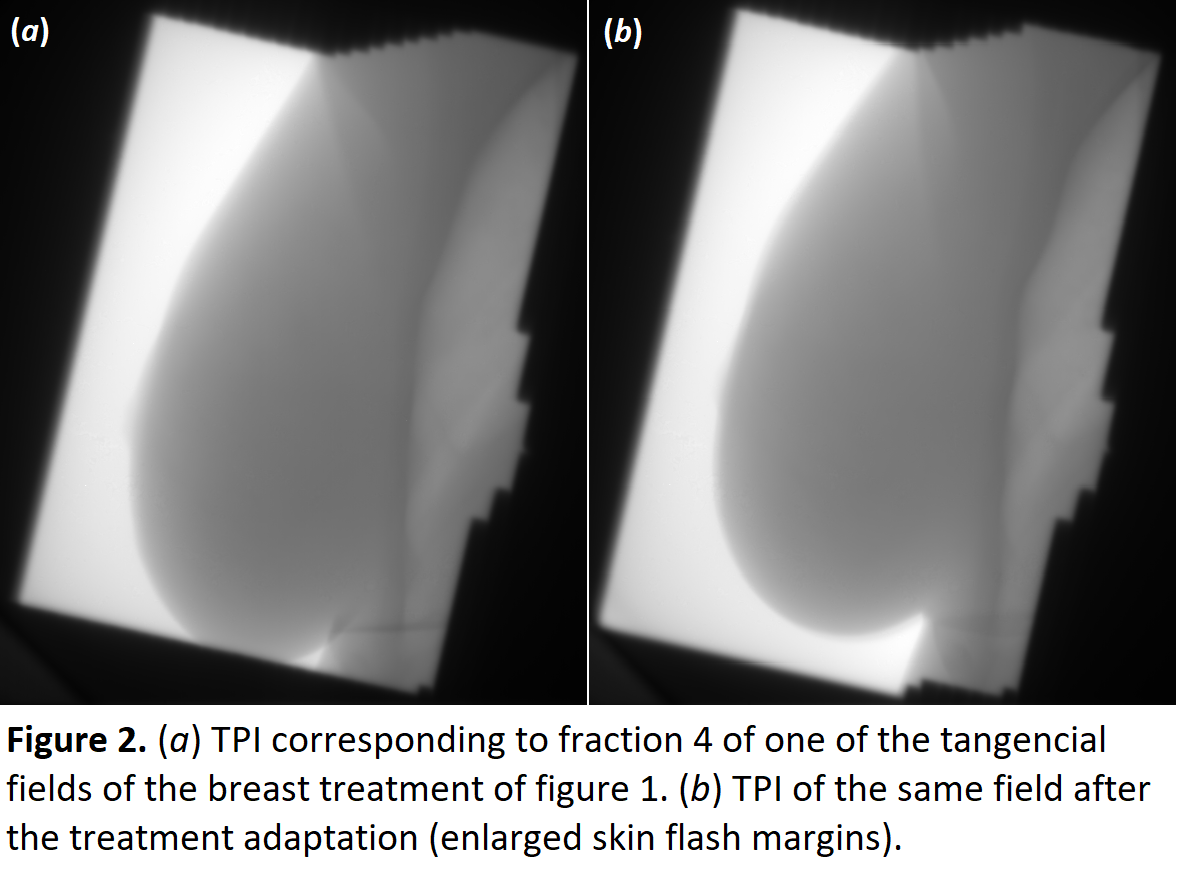
The TPIs provided a reliable assessment of the daily variability of the patient position. As an example, a remarkable craneocaudal position drift was detected for a given patient by the TGRT technique (figure 1). A visual inspection of the treatment fields (figure 2a) confirmed this finding triggering a treatment adaption. As a result, fields with enlarged skin-flash margins were planned (figure 2b).
Conclusion
The TGRT is a technically feasible technique in all radiotherapy facilities after minimally adapting the institutional clinical workflow. Treatment time and patient safety are not impaired. At this stage, the TGRT technique quantifies position errors and adds patient monitoring capabilities that can lead to treatment adaption.