Arc proton therapy for esophageal cancer: feasibility and first plan comparison with IMPT
PO-1963
Abstract
Arc proton therapy for esophageal cancer: feasibility and first plan comparison with IMPT
Authors: Macarena Chocan1, Hamdiye Ozan1, Anne Catherine Wera1, Sophie Wuyckens1, Erik Engwall2, Viktor Wase3, Otte Marthin2, Johan Sundström3, Ana Barragan1, John A. Lee1, Edmond Sterpin1
1UCLouvain, MIRO, Brussels, Belgium; 2RaySearch Laboratories , Research and Development, Stockholm, Sweden; 3RaySearch Laboratories, Research and Development, Stockholm, Sweden
Show Affiliations
Hide Affiliations
Purpose or Objective
Arc proton therapy (ArcPT) appears as an alternative to IMPT due to its capability to improve dose conformality, while reducing both the treatment time and the probability of normal tissue complications (NTCP) for several tumor locations, such as lungs, breast, brain, head and neck, and prostate. This work aims to study the feasibility and performance of ArcPT against IMPT in esophageal cancer, for which no results have been reported yet, and to analyze potential benefits and pitfalls of ArcPT for this tumor location.
Material and Methods
Dynamic ArcPT plans were created for a database of 20 patients with a dedicated optimization algorithm (1) in a research version of RayStation 12A, following the clinical goals established in the PROTECT clinical trial (prescription of 50.4Gy). A beamset of 2 entangled arcs in opposing rotation, 1 revolution each, and 2° angular spacing was used. The arc range was set to 80-200° (Fig 1a). Robust optimization was performed simulating 7 mm setup and ±2.6% range error. In total, 28 scenarios were later evaluated. Conventional IMPT plans were also generated for each patient, using 2 posterior oblique beams (Fig 1b). All IMPT plans were clinically approved by an experienced physician. ArcPT and IMPT plans were compared in terms of clinically relevant dose-volume metrics, in both the nominal and worst-case scenarios, for the target volume and main organs at risk (OARs). Body integral dose and NTCP for lung toxicity (2) were also assessed.
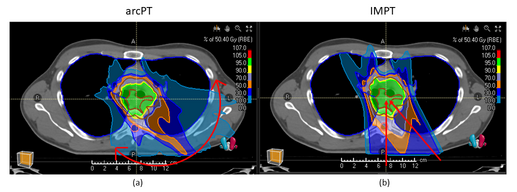
Figure 1. Beam configuration: (a) arcPT (b) IMPT
Results
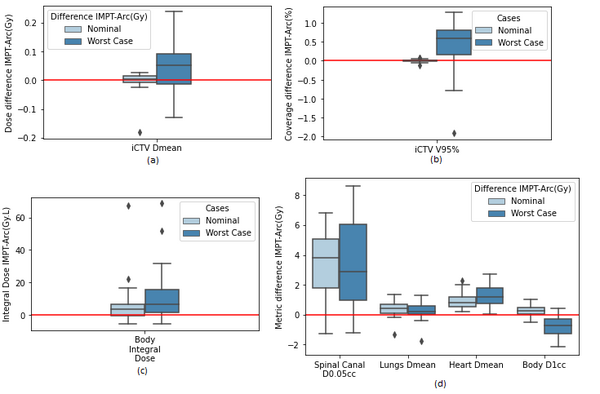
Figure 2. For 20 patients, (nominal/worst-case scenarios): (a) and (b) Difference in D mean/V95% for iCTV. (c) Difference in integral dose to the full body volume (d) Difference in relevant metrics OARs.
Target coverage was equivalent for both modalities (no significant difference, p > 0.05, for V95% and D mean), considering nominal and worst-case scenarios (Figure 1a,1b). However, arcPT managed to slightly decrease the integral body dose (median difference equal to 5Gy, p = 0.015) and the dose to some relevant OARs in the nominal case, like lungs (median ΔDmean = 0.45 Gy, p= 0.002) and heart (median ΔDmean = 0.8 Gy, p = 1.9e-06). The largest improvement was seen in the spinal canal, where arcPT plans decreased median D0.05cc by 4Gy. Similar trends are observed for the worst-case scenario (Heart ΔDmean = 1.2 Gy, p =1.9e-06, Lungs ΔDmean = 0.23 Gy, p = 0.02), indicating that the plans are robust against setup/range errors. For arcPT, the worst-case median body D1 is about 1Gy larger, which might be a sign of lower robustness in terms of hot spots. Regarding ΔNTCP (IMPT-arcPT) for lung toxicity, arcPT showed an average decrease of (0.7 ± 1) % [range –1.8 to 2.6%].
Conclusion
ArcPT can preserve and slightly improve IMPT benefits for esophageal cancer in terms of target coverage and OAR sparing, while potentially decreasing lung toxicity. Further investigation is needed to assess potential advantages in treatment time.
(1) Engwall et al. 2022 (2) Thomas et. al 2019