Impact of Uncertainties in Robust Optimization for Head and Neck Intensity Modulated Proton Therapy
PO-1952
Abstract
Impact of Uncertainties in Robust Optimization for Head and Neck Intensity Modulated Proton Therapy
Authors: Nesrin Dogan1, Kyle Padgett2, Michael Butkus3, Yihang Xu2
1University of Miami, Radaition Oncology, Miami, USA; 2University of Miami, Radiation Oncology Department, Miami, USA; 3University of Miami, Radiation Oncology, Miami, USA
Show Affiliations
Hide Affiliations
Purpose or Objective
Intensity-modulated proton therapy (IMPT) dose distributions for head and neck cancer are sensitive to uncertainties in patient setup and proton range. Robust optimization (RO) which can account for these uncertainties generate high quality treatment plans that remain acceptable under such uncertainties. The objective of this study was to assess the impact of the degree of robustness on target coverage and organ at risk (OAR) doses under both systematic setup and range uncertainties for head and neck IMPT plans.
Material and Methods
Five patients with head and neck cancer and treated with IMPT were included. The prescription doses to Clinical Target Volumes (CTVs) were: CTVprimary:70Gy, CTVsecondary:60Gy and CTVtertiary:54Gy. The plan was delivered in 35 fractions utilizing a simultaneous integrated boost technique. The OARs included were spinal cord, brainstem, parotids, cochlea, constrictors, esophagus, and larynx. For each patient, a proton multifield optimization plan was created with an arrangement of 3 or 5 fields depending on target extent and surrounding anatomy. The relative biological effectiveness of 1.1 was used for the weighted dose. During RO-IMPT, the targets were the only structures that were selected to be robustly optimized with the objective to cover the 95% of each CTV volume with 100% of the prescription dose. For each patient, setup uncertainties varied from ±1mm to ±7mm and along with proton range uncertainties changing from ±1% to ±7%. The worst-case scenario was required to achieve V95 > 95% for CTV while keeping the OAR constraints as low as possible. The plans were assessed for target coverage, and dose-volume constraints for OARs, including NTCPs for dysphagia, xerostomia, and larynx edema.
Results
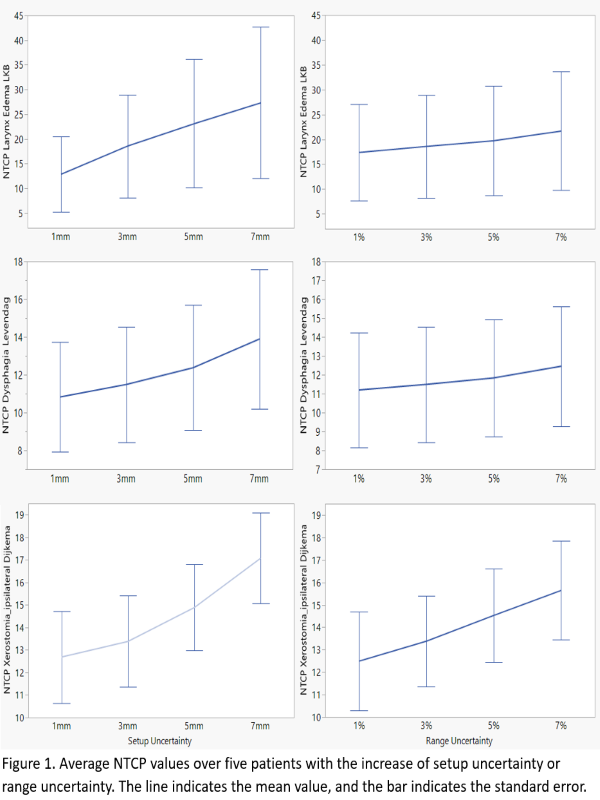
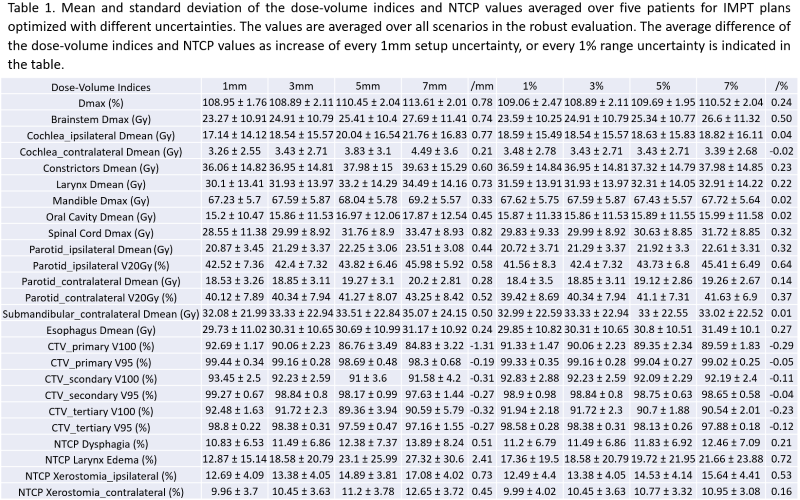
The average increase in mean dose for each 1mm of increased setup uncertainty for constrictors, larynx and ipsilateral cochlea are 0.6Gy, 0.73Gy and 0.77Gy with the increase of setup uncertainty from 1mm to 7mm. The average increase in maximum dose for each 1mm of increase of setup uncertainty for brainstem and spinal cord is also increased by 0.74Gy and 0.82Gy with the increase of setup uncertainty from 1mm to 7mm. A reduction of every 1mm on setup uncertainty also results in the average reduction of the NTCP values for dysphagia, larynx edema and ipsilateral parotid xerostomia of 0.51%, 2.41% and 0.73% respectively. Decreasing range uncertainty on the dose-volume indices and NTCP values has resulted in much smaller impact than decreasing setup uncertainty, with an average reduction of NTCP value on dysphagia, larynx edema and ipsilateral parotid xerostomia 0.21%, 0.72% and 0.53% respectively when the range uncertainty is decreased each 1% (see Table 1 and Figure 1).
Conclusion
This study demonstrated that varying the degree of setup uncertainty had a significantly larger impact than varying the range uncertainty for head and neck cancer patients, implying clinically significant impact for bilateral head and neck cases.