Combined proton-photon radiotherapy for prostate cancer using a horizontal fixed proton beamline
PO-1950
Abstract
Combined proton-photon radiotherapy for prostate cancer using a horizontal fixed proton beamline
Authors: Louise Marc1, Krishna P Subedi1,2, Gieri Candinas1, Silvia Fabiano1, Antony J Lomax3,2, Jan Unkelbach1
1University Hospital Zurich, Radiation Oncology, Zurich, Switzerland; 2ETH Zurich, Physics, Zurich, Switzerland; 3Paul Scherrer Institute, Center for Proton Therapy, Villigen, Switzerland
Show Affiliations
Hide Affiliations
Purpose or Objective
Objective: Proton therapy is a limited resource, mainly due to the high cost and bulkiness of the proton gantry. Integrating a horizontal fixed proton beamline (FBL) into a conventional treatment room with a Linac and a robotic couch, allowing protons and photons to be delivered in the same fraction, might increase the availability of proton therapy. This concept is studied for prostate cancer including nodal irradiation.
Material and Methods
Methods: The optimal combined proton-photon treatment (CPPT) is determined through simultaneous optimization of the cumulative physical dose using a hybrid robust planning approach (a PTV margin for setup/motion and a probabilistic approach for range uncertainties of +/- 3.5%). Photons are delivered with a full VMAT arc, and for IMPT 4 beams in the coronal plane are used. Three patients in supine position are considered. Planning objectives are to deliver 57.75 Gy to the prostate and 45 Gy to the nodal target, achieve conformity, and minimize the mean dose to the bladder, rectum and remaining healthy tissue.
Results
Results: Compared to VMAT-only treatments, CPPT reduces the mean dose to the normal tissue for all three patients. For patient 1, the mean dose is reduced from 24.6 Gy to 21.8 Gy (bladder), from 25.1 Gy to 22.6 Gy (rectum), and from 6.5 Gy to 4.7 Gy (healthy tissue). In CPPT, on average, protons and photons contribute approximately the same amount of dose to the target volume. For instance, for patient 1, the mean dose delivered to the target volume is 24.4 Gy for the proton contribution and 23.6 Gy for the photon contribution. Photons are mainly delivered through anterior and posterior beams, which are not deliverable with an FBL in lying position. In particular, photon beams are used to improve the conformity and robustness of the dose distribution at the interface of prostate and rectum (Figure 1). Thereby, CPPT improves treatment plan quality compared to IMPT-only treatments as shown in the DVH robustness analysis in Figure 2 for patient 1. More precisely, for IMPT-only, the mean rectum dose is 27.8 Gy in the nominal scenario and further increased for range overshoot (red dashed line). Furthermore, the target is underdosed for IMPT-only treatment in the case of a range undershoot (red dotted line), which can be avoided with CPPT (blue dotted line). Similar results were obtained for patients 2 and 3.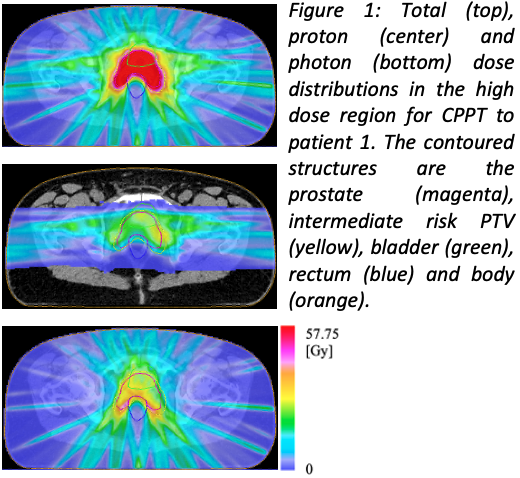

Conclusion
Conclusion: CPPT with an FBL may make proton therapy available to a larger patient population including prostate cancer patients. It may reduce normal tissue dose compared to VMAT-only treatments, and may improve conformity and robustness compared to IMPT-only treatments.