Visual outcome after fractionated stereotactic radiotherapy for optic nerve sheath meningioma
Buket Kinaci-Tas,
The Netherlands
PO-1153
Abstract
Visual outcome after fractionated stereotactic radiotherapy for optic nerve sheath meningioma
Authors: Buket Kinaci-Tas1
1Leiden University Medical Centre, Radiotherapy, Leiden, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
Optic nerve sheath meningiomas (ONSMs) are rare benign neoplasms of the orbita and occur primarily in adults with a peak incidence in the 45 to 55 years old age group. The triad of progressive visual loss, optic disc pallor, and retinochoroidal shunting is typical for ONSM. The triad occurs relatively late and is seen in 25-33% of the patients. A ‘tram tracking sign’ can be seen on magnetic resonance imaging and is suggestive for ONSM. Invasion into surrounding orbital structures is rare, contributing to an excellent prognosis for life. The mass effect leads to compression of the optic nerve and deterioration of the optic nerve function with loss of visual acuity (VA), and diminished visual fields. Radiotherapy has proven to be the only treatment modality allowing stabilization of the tumor and even improvement of VA in 25-80% of the patients. Acute radiotherapy induced ocular toxicities (conjunctivitis, dry eye) are well known, but the long-term ocular toxicity retinal vasculopathy, which may contribute significantly to a deterioration of patient’s visual function and quality of life (QoL), is less known. We primarily aimed to evaluate the visual outcome (VA, visual field (VF), and color vision (CV)) after radiotherapy), and secondary the occurrence of retinal vasculopathy through qualitative and quantitative analysis and study how these interfere with QoL.
Material and Methods
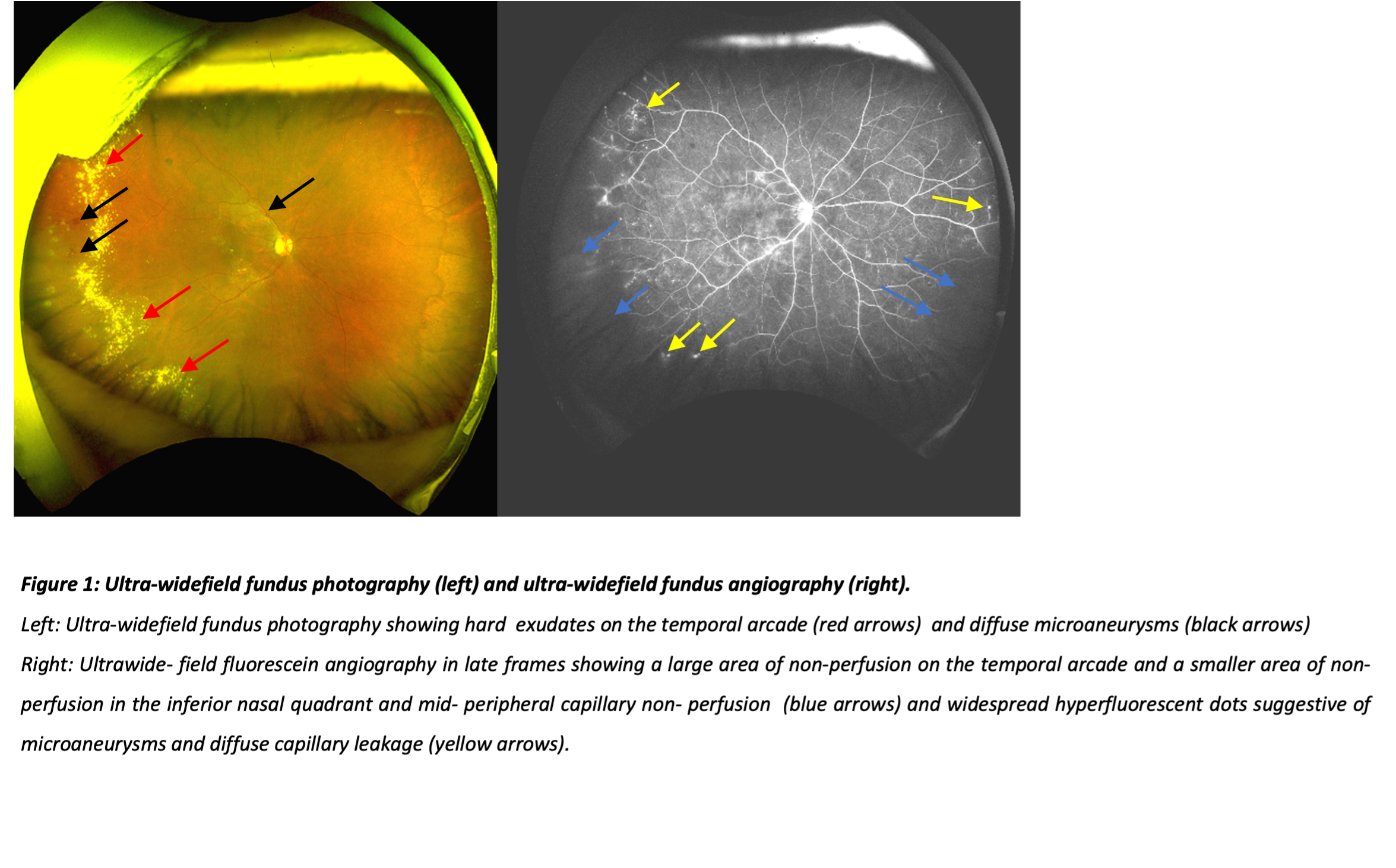
Adult patients who had fractionated stereotactic radiotherapy (54Gy total dose given in 30 fractions of 1.8Gy) for ONSM with a follow-up of at least 18 months were invited for a detailed ophthalmological assessment. VA, VF, and CV were tested which together represented the visual outcome (i.e. our primary parameter). The secondary outcome parameter was the occurrence of retinal vasculopathy. Ultra-widefield fluorescein angiography (UWFA) was performed for qualitative evaluation of the superficial retinal vasculature and optical coherence tomography angiography for quantitative evaluation of the retinal microvasculature. Additionally, we analyzed how these interfere with QoL through ‘the Graves’ ophthalmopathy QoL questionnaire.
Results
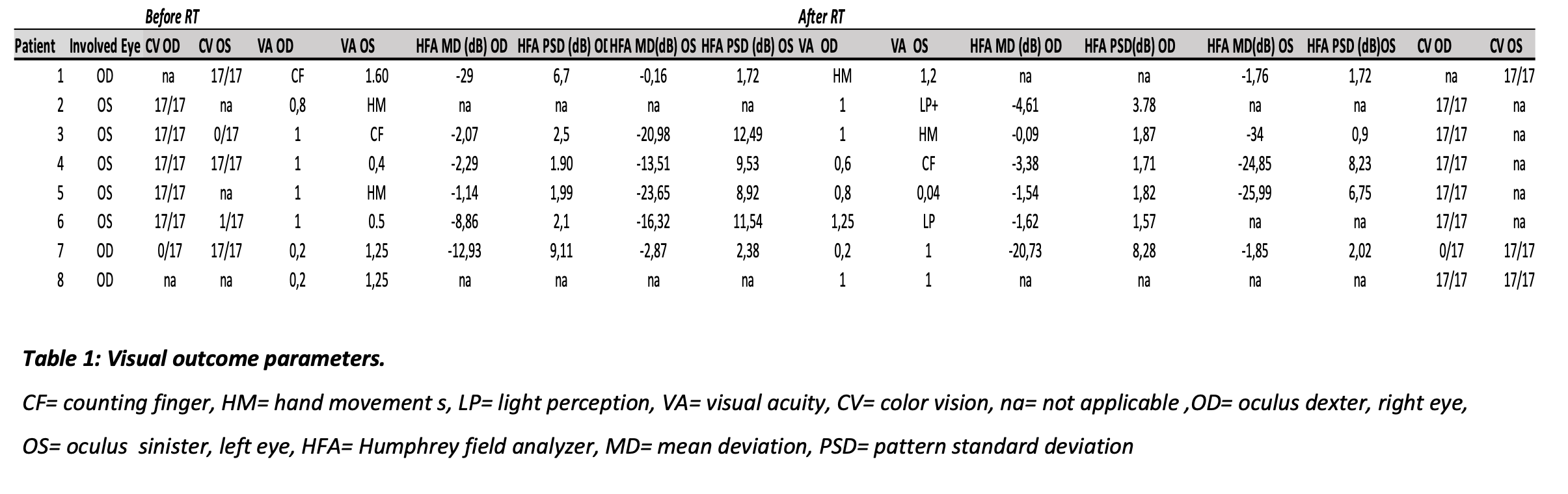
Eight patients were included. VA improvement occurred in 13%, stabilization in 13%, and deterioration in 74%. VF deterioration was observed in 75% and stabilization in 25%. CF improvement occurred in 12%, stabilization in 63%, and improvement in 25%. (Table 1) Capillary nonperfusion and microaneurysms were observed on UWFA indicating retinal vasculopathy in two patients (Figure 1). In patients with exophthalmos induced by the tumor, 36% felt their condition had influenced their self-confidence.
Conclusion
Fractionated stereotactic radiotherapy for ONSM yields positive results for VA and VF in patients with a good vision at the start of the treatment. Therefore, starting radiotherapy before severe VA loss occurs, could be beneficial to preserve visual function. The change in appearance due to exophthalmos was a serious QoL impairment.