Stereotactic re-irradiation of relapsed intracranic lesions: a monoinstitutional experience
PO-1129
Abstract
Stereotactic re-irradiation of relapsed intracranic lesions: a monoinstitutional experience
Authors: Chiara Chissotti1,2, Miriam Torrisi1,2, Andrei Fodor1, Chiara Lucrezia Deantoni1, Sara Broggi3, Federica Ferrario1,2, Laura Giannini1,2, Stefano Lorenzo Villa1,1, Martina Midulla1,1, Carmen Rosaria Gigliotti3, Italo Dell'Oca1, Roberta Castriconi3, Flavia Zerbetto1, Claudio Fiorino3, Antonella Del Vecchio3, Stefano Arcangeli4,2, Nadia Gisella Di Muzio1,5
1IRCCS San Raffaele Scientific Institute, Department of Radiation Oncology, Milan, Italy; 2Università degli Studi di Milano Bicocca, School of Radiation Oncology, Milan, Italy; 3IRCCS San Raffaele Scientific Institute, Medical Physics, Milan, Italy; 4ASST Monza, Department od Radiation Oncology, Monza, Italy; 5Università Vita-Salute San Raffaele, Medicine and Surgery, Milan, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
Recurrent primary brain tumors or metastases (mts) are challenging and stereotactic re-irradiation is increasingly used as a salvage treatment. Here we report the experience of our Institute with stereotactic reirradiation in pts with intracranial recurrence.
Material and Methods
From 1/2018 to 7/2022, 161 lesions in 42 patients (pts) were re-irradiated with robotic SRT (Cyberknife®, CK). Primary tumor was NSCLS for 13 pts, breast cancer for 12, glioblastoma for 5, meningioma for 3, melanoma for 2, hemangiopericytoma for 2, oligodendroglioma for 2, pituitary adenoma for 2, prostate cancer for 1 patient. Previous RT on the same volume was performed with: Gamma Knife in 10 pts, whole-brain RT in 10, CK in 10, post-operative IMRT in 5, VMAT SRT in 4, and post-operative 3D-CRT in 3 pts. Median time from previous RT was 13 (3-378) months. Eight pts had ≥2 previous treatments. Median GTV was 6.9 (0.02-78.32) cc. Median PTV was 12 (0.07-136.9) cc. Median prescribed dose was 30 (21-35) Gy in 1-5 fractions, at a median isodose of 70 (69-80)%. Prophylactic corticosteroid therapy was prescribed to all pts. Post-treatment MRI was used to assess response to re-irradiation. Survival curves were calculated from the date of treatment by using the Kaplan-Meier (KM) method.
Results
Median follow-up after re-irradiation was 10 (2.8-39.7) months. SRT was delivered on a median number of 1 (1-24) lesions; 8 pts were treated on >5 lesions simultaneously (from 6 to 24 lesions). Acute toxicity was G2 headache in 3 pts: (with GTV >1cc or >3 lesions), treated by increasing the dose of corticosteroids. Radionecrosis occurred in 3 pts: 1 patient (GTV 1.38 cc) underwent 2 previous VMAT SRT and presented seizures, 1 patient (GTV 0.49 cc) underwent 1 previous VMAT SRT and presented headache and 1 patient (GTV 5.54 cc) underwent previous GK and CK and was asymptomatic. Maximal local response, evaluable in 35 pts, was: complete response (RC) in 2 patients, partial response (PR) in 20 pts, stable disease (SD) in 7 pts and progressive disease (PD) in 6 pts. Six-, 12- and 18 month overall survival were 76.9%, 51.8% and 34.2% (see Fig.1). Six-, 12- and 18 month local relapse-free survival (LRFS), evaluable in 32 pts, were 70.9%, 55.6%, 55.6%.
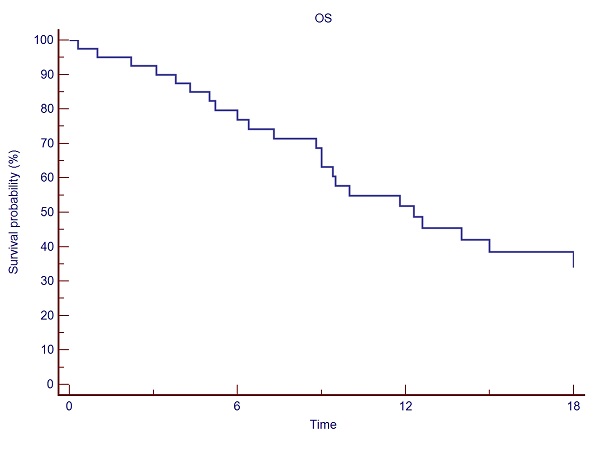
Fig.1: Six-, 12- and 18 month overall survival
Conclusion
SRT re-irradiation of brain recurrent disease is effective with responses in 83% of pts. Accurate patient selection is warranted in order to avoid toxicity and a longer follow-up is needed to confirm these results.