A novel tool to evaluate and quantify radiation induced lung injury(RILI): volume of pneumonia patch
Yihui Lin,
Taiwan, Province of China
PO-2322
Abstract
A novel tool to evaluate and quantify radiation induced lung injury(RILI): volume of pneumonia patch
Authors: Jing Wen Huang1,2, Yi Hui Lin1, Yu Tuan3, Jia Fu Lin1, Yu Wei Hsu4, Ting Na Wei1
1Taichung Veterans General Hospital, Department of Radiation Oncology, Taichung, Taiwan; 2National Chung Hsing University, Institute of Biomedical Sciences, College of Life Sciences, Taichung, Taiwan; 3Taichung Veterans General Hospital, Department of Psychiatry, Taichung, Taiwan; 4Taichung Veterans General Hospital, Cancer Prevention and Control Center, Taichung, Taiwan
Show Affiliations
Hide Affiliations
Purpose or Objective
In lung cancer, radiation induced lung injury (RILI), or radiation pneumonitis (RP) was our most concern issue after radiotherapy. We investigated the correlation between (1) Dose-Volume-Histogram (DVH), (2) volumes of radiation pneumonitis lesions and (3) radiation pneumonitis grades after radiotherapy.
Material and Methods
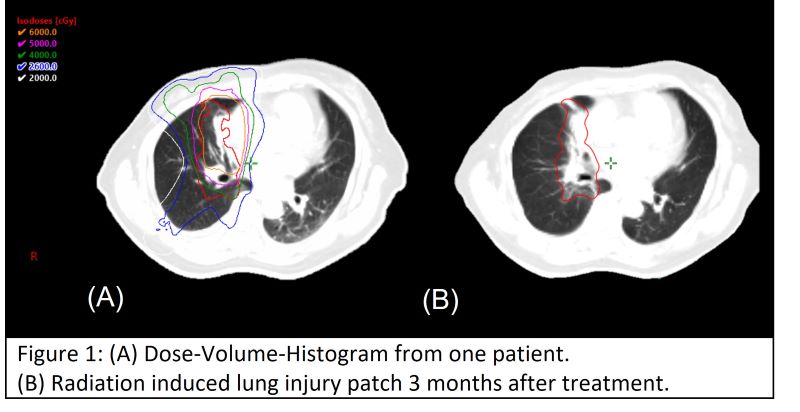
We retrospectively collected patients of non-small lung cancer who underwent curative radiation dose to thorax without receiving chest radiotherapy before this treatment course. Post treatment CT images were imported into treatment planning system (TPS) to evaluate correlation of dosimetry parameters and volume of pneumonia patch by using deformable image registration. The DVH and RILI patch contour demonstrated in (Figure 1)
Results
From 2019/01/01 to 2020/12/30, total 71 non-small cell lung cancer patients with 169 CT scans met our criteria. We have three important findings.
(1) In all patient group, we found that volume of radiation pneumonitis (RPv) max and RP grade max was statistically significant (p<0.001).
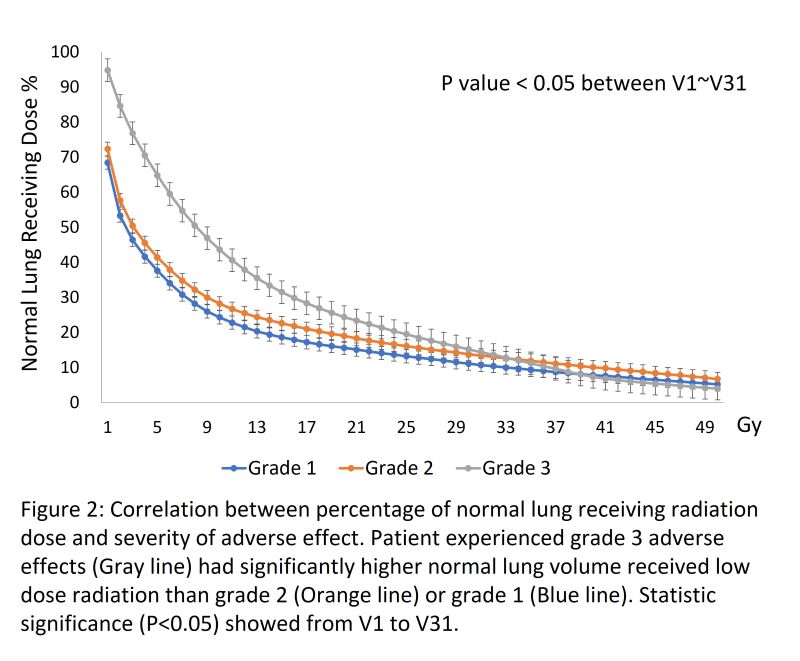
(2) The DVH parameters also affect radiation pneumonitis severity. We found that mean lung dose (MLD), and percentage of normal lung receiving dose, between 1 Gy (V1) to 31 Gy (V31) was significantly correlated to RP.
(3) If volume of radiation pneumonitis account for a small percentage of lung, patient may experience no symptoms. We found that cut-off point for symptom occurrence was 4.79% RPv in total lung volume. For this cut-off, the area under the curve (AUC) was 0.779. In the groups with grade 1 and grade 2 radiation pneumonitis, it was found that the radiation dose of 2600cGy covered ≥80% of radiation pneumonitis lesions in more than 80% patients.
Conclusion
The percentage of radiation pneumonitis lesion volume to total lung volume is a good indicator for quantifying radiation pneumonitis. Radiation pneumonitis lesions can be projected onto the original radiotherapy plan using coverage of 26Gy isodose line to determine whether radiation induced lung injury.
This work was supported in part by the National Science and Technology Council, Taiwan under Grant of NSTC 111-2634-F-006-012