Internal guidelines to reduce lymph-node contour variability for total marrow/lymph node irradiation
PO-2355
Abstract
Internal guidelines to reduce lymph-node contour variability for total marrow/lymph node irradiation
Authors: Damiano Dei1, Nicola Lambri2, Leonardo Crespi3, Ricardo Coimbra Brosio3, Daniele Loiacono3, Marta Scorsetti4, Pietro Mancosu5
1Humanitas Research Hospital, Humanitas University, Radiotherapy, Rozzano, Milano, Italy; 2Humanitas University, Department of Biomedical Sciences, Rozzano, Milano, Italy; 3Politecnico di Milano, Dipartimento di Elettronica, Informazione e Bioingegneria, Milano, Italy; 4IRCCS Humanitas Research Hospital, Humanitas University, Radiotherapy, Rozzano, Milano, Italy; 5IRCCS Humanitas Research Hospital, Medical Physics Unit, Rozzano, Milano, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
Total marrow/lymph node irradiation (TMI/TMLI) is a modulated radiotherapy technique for delivering full dose to the hematological target and sparing the dose from organs at risk (OARs) within the conditioning regimen before bone marrow transplantation. The TMI/TMLI target includes the whole bones, lymph-node system, and spleen. In particular, the lymph-node chains delineation is the most demanding contouring. We evaluated the impact of introducing internal contouring guidelines to reduce the inter- and intra-variability of lymph-node contour in TMI/TMLI.
Material and Methods
Since 2010, 114 patients were treated in our center with TMLI using volumetric modulated arc therapy (VMAT). Ten patients were randomly selected from the internal database. The lymph-nodes clinical target volume (CTV_LN) was re-contoured according to new internal guidelines (GL) by a single expert radiation oncologist (CTV_LN_GL_RO1), and compared to the historical one (CTV_LN_Old). The guidelines efficacy in reducing inter- and intra-variability was prospectively evaluated in, respectively, six and four patients. The CTV_LN was splitted in four regions (H&N, Thoracic, Abdominal, and Pelvic areas) for better evaluate the agreement. Dice similarity coefficient (DSC) was calculated for all paired contours. Planning target volume (PTV_LN) was generated adding an isotropic margin of 5 mm to the CTV_LN. The TMI/TMLI plans were optimized on PTV_Tot (=PTV_bones+PTV_LN+PTV_spleen) using PTV_LN_old for retrospective patients and PTV_LN_RO1 for prospective patients. The volume received by the 95% of the prescription dose (V95%) were computed for all contours to assess the target coverage and guidelines consistency.
Results
A total of 250 target volumes were considered. Median CTV_LN and PTV_tot were, respectively, 2100±610 cm3 and 16221±2587 cm3. The mean DSCs were 0.82±0.09, 0.97±0.01, and 0.98±0.02 for, respectively, CTV_LN_Old vs. CTV_LN_GL_RO1, GL inter- and intra-variability (figure 1, 2)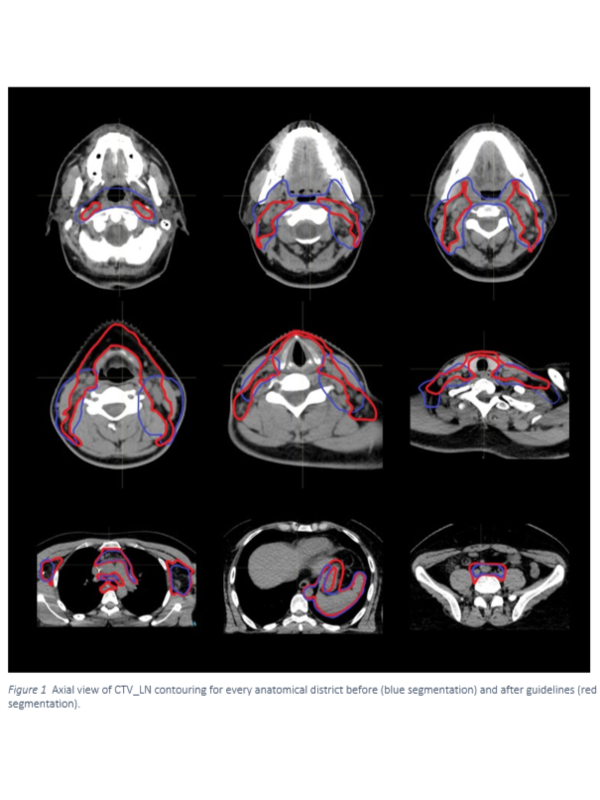
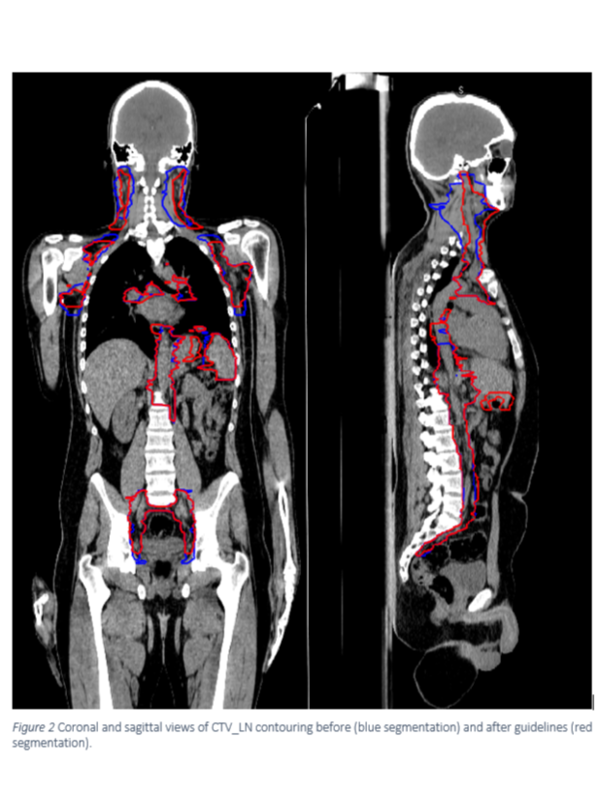 . The largest and lowest differences were observed in, respectively, H&N and abdomen regions. Mean V95% dose differences were 4.8±4.7%, 0.3±0.5%, and 0.1±0.1%, for the same couples.
. The largest and lowest differences were observed in, respectively, H&N and abdomen regions. Mean V95% dose differences were 4.8±4.7%, 0.3±0.5%, and 0.1±0.1%, for the same couples.
Conclusion
The efficacy of internal guidelines in reducing the CTV_LN inter- and intra-variability was demonstrated. The high target coverage agreement of CTV_LN_Old vs. CTV_LN_RO1 revealed the historical CTV-to-PTV margins to be safe even if relatively low DSC was observed. The introduction of GL increased the CTV dose coverage could allow margin reduction.