Should we limit the maximum dose in inverse-planning-based lung SBRT plans?
PO-2332
Abstract
Should we limit the maximum dose in inverse-planning-based lung SBRT plans?
Authors: Cristina Castro1, Elisabet Escudero2, Carla Cases1, Francesc Casas1, Gabriela Antelo1, Meritxell Mollà1
1Hospital Clínic de Barcelona, Oncologia Radioteràpica (ICMHO), Barcelona, Spain; 2Hospita Clínic de Barcelona, Oncologia Radioteràpica (ICMHO), Barcelona, Spain
Show Affiliations
Hide Affiliations
Purpose or Objective
In lung SBRT, the inverse planning process can lead to undesired fluence peaks between the ITV and PTV to compensate the lack of lateral equilibrium and a low density tissue. On one hand, the use of more advanced calculation engines in the optimization process, further increases this effect. On the other hand, when using modulated delivery techniques, the desired steep dose gradient is no longer directly correlated with the presence of large maximum doses within the PTV.
The purpose of this study is to analyze the impact of the basic optimization parameters prevalent in this treatment, and asses its impact independently.
Material and Methods
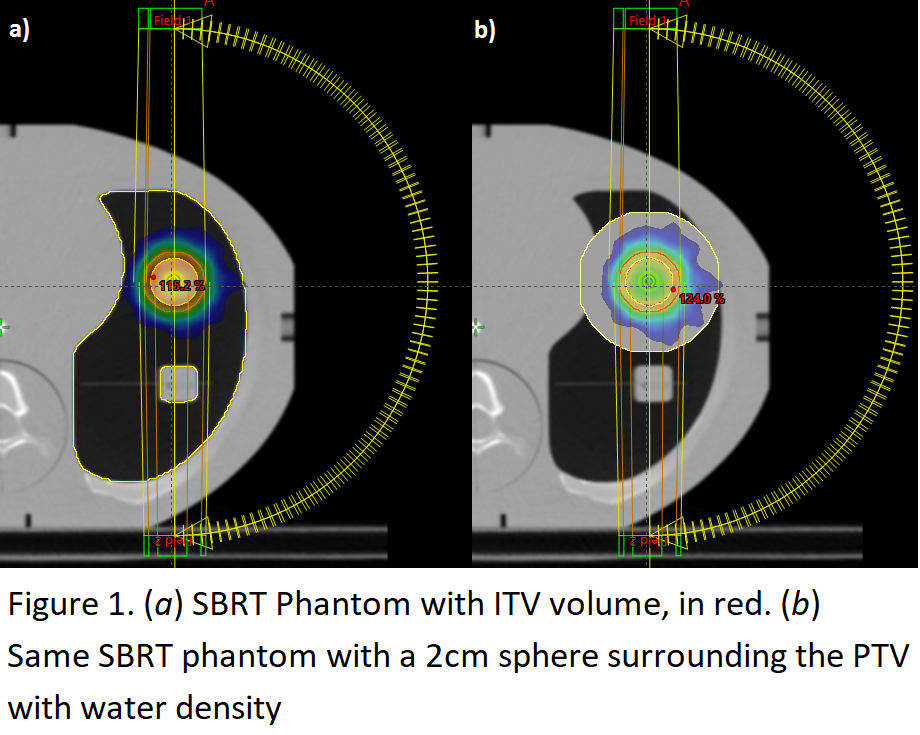
We optimized and calculated 51 VMAT treatment plans (Eclipse v 16.1, PO, Acuros TPS, dose to medium) using a SBRT lung phantom (CIRS) with the Hounsfield Units (HU) of the ITV overridden with water (Figure 1a). The variables in the optimization process were:
- Maximum PTV dose: 105%, 110%, 115%, 120% of the prescribed dose.
- Maximum dose priorities: 0, 50, 100, 150, 200.
- NTO priorities: 0, 100, 200.
For each plan the optimization process was started with a specific combination of parameters and remained unmodified and calculating the intermediate dose. For all cases the dose was normalized to ensure that the 100% isodose covered 95% of the PTV.
The analyzed dosimetric parameters were:
- Mean dose to the ITV D_meanITV
- Mean dose to a ring enclosing 0.5 cm (D_mean0.5) beyond the PTV and 1.5 cm (D_mean1.5) beyond the PTV, excluding the first 0.5 cm.
- Mean dose to the ITV to PTV ring, calculated in a phantom with a 2 cm sphere surrounding the PTV with water HU (Figure 1b) (D_meanP-I).
The last parameter was used, compared to D_meanITV to evaluate the fluence peaks.
We also defined Dmax strength as the Dmax objective priority divided by the difference between the Dmax value and the prescribed dose.
Results
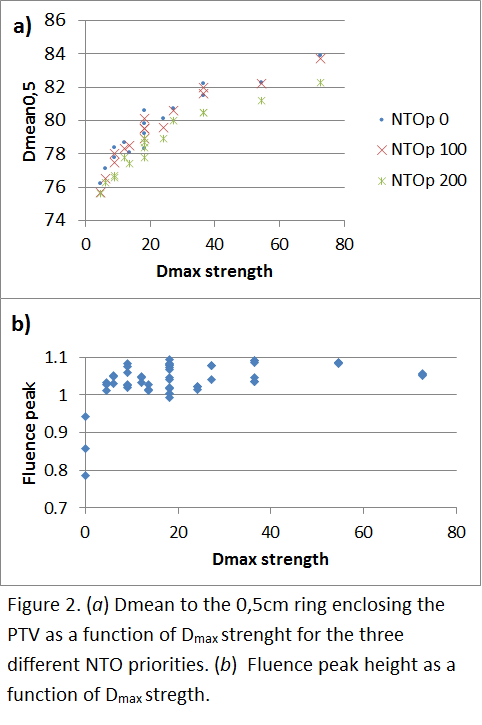
We have observed that the use of the NTO with a high priority improves the dose gradient beyond the PTV independently of Dmax and its priority. Conversely, the use of a low Dmax, independently of the priority assigned, has a negative impact on the dose gradient. The worsening of the gradient is more affected by the use of a Dmax, than by the priority on the NTO (Figure 2a).
As expected, the use of a Dmax objective reduces the mean dose to the ITV, but this reduction occurs even with low priorities, and it is maintained almost constant with increasing priorities.
The presence of fluence peaks also increases with lower values of the Dmax objective. When evaluating Dmax strength we see that this effect is true for the cases when Dmax priority is zero, as soon as the Dmax priority is increased the fluence peaks appear and remain almost constant (Figure 2b).
Conclusion
Although the use of Dmax in the optimization in lung SBRT may help to deliver more congruent doses to the ITV among different centers or patients, its use has a negative impact on the dose gradient and the magnitude on fluence peaks.