Dosimetric impact of tumour rotation in real-time adaptive liver stereotactic body radiation therapy
Chandrima Sengupta,
Australia
PO-1896
Abstract
Dosimetric impact of tumour rotation in real-time adaptive liver stereotactic body radiation therapy
Authors: Chandrima Sengupta1, Doan Nguyen1, Trevor Moodie2, Simon Skouboe3, Thomas Ravkilde4, Per Poulsen4, Ricky O' Brien1, Jeremy Booth5, Tim Wang2, YooYoung Lee6, Paul Keall1
1Image X Institute, University of Sydney, Faculty of Medicine and Health, Sydney, Australia; 2Crown Princess Mary Cancer Center, Department of Radiation Oncology, Sydney, Australia; 3Danish Center for Particle Therapy, Department of Oncology , Aarhus, Denmark; 4Aarhus University Hospital, Department of Oncology, Aarhus, Denmark; 5Northern Sydney Cancer Center, Department of Radiation Oncology , Sydney, Australia; 6Princess Alexandra Hospital, Department of Radiation Oncology , Brisbane, Australia
Show Affiliations
Hide Affiliations
Purpose or Objective
In liver stereotactic body radiation therapy (SBRT), intra-fraction tumour translation deteriorates the planned dose distribution [1]. Most of the major advances in motion management to date have focussed only on this one aspect of tumour motion, translation. However, large intra-fraction liver tumour rotation up to 15º has been observed [2-5]. As technological innovation evolves towards delivering increasingly precise radiotherapy, it is important to investigate the dosimetric impact of intra-fraction tumour rotation in liver SBRT treatments. In this study, we quantified the dosimetric impact of intra-fraction liver tumour rotation for seven liver cancer patients treated in the TROG 17.03 LARK clinical trial [6].
Material and Methods
Patients received SBRT in one of three treatment schedules: 3x17 Gy, 5x10 Gy, 5x6.5 Gy. The patients were treated at breath-hold using 6FFF VMAT plans with a 5 mm gross tumour volume (GTV) to planning target volume (PTV) margin. The intra-fraction tumour translation and rotation was measured with Kilovoltage Intrafraction Monitoring (KIM) [7]. A gating threshold of 3 mm for 5 sec or 5 mm for 5 sec was used in KIM. The residual translation is denoted as Tres. Intra-fractional rotation (Runcorr) remained uncorrected during treatment. The delivered dose was reconstructed including intra-fractional dynamic (a) translation and rotation (Tres+Runcorr) and (b) only translation (Tres) using the DoseTracker software [8-9]. The differences from the planned dose including translation, Tres and rotation, Runcorr (ΔD(Tres+Runcorr)) and including only translation, Tres (ΔD(Tres)) were determined for GTV D100 and PTV D95.
Results
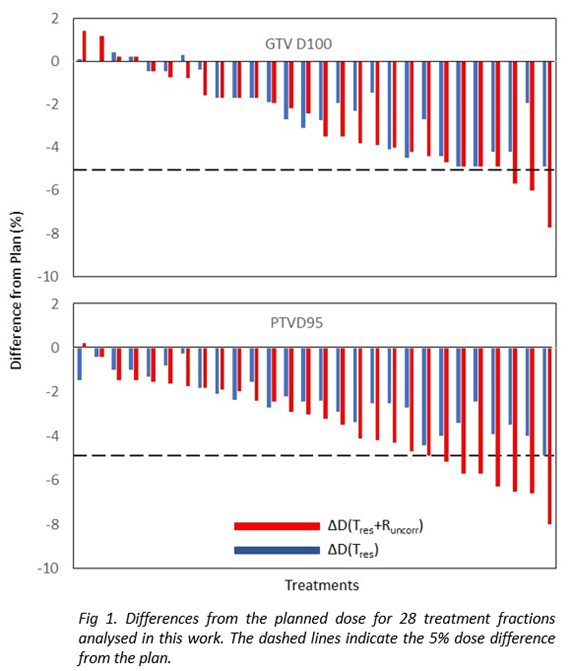
The mean and standard deviation of translation (Tres) and rotation (Runcorr) in left-right, superior-inferior and anterior-posterior directions were 0.5±1.0, 0.3±1.6, -0.6±1.4 mm and 0.0±2.6º, 1.4±2.4º, 1.6±2.1º respectively over all treatment fractions for all patients, the minimum and maximum rotation angles being -21.9º and 17.9º respectively. ΔD(Tres +Runcorr) was >5% in 3 fractions (11%) for GTV and in 7 fractions (25%) for PTV out of 28 treatment fractions (Fig.1). ΔD(Tres) was always within 5% of the planned dose in all treatment fractions for both GTV and PTV. The cumulative dose (ΣD(Tres +Runcorr) and ΣD(Tres)) over all treatment fractions for all patients was always within 5% of the planned dose for both GTV and PTV.
Conclusion
The dosimetric impact of intra-fraction liver tumour rotation during liver SBRT treatments was quantified for the first time in this study. These results suggest that while dose errors > 5% exist in certain fractions due to residual translation (Tres) and uncorrected rotation (Runcorr), the cumulative dose for every patient remains within 5% of the planned dose. Residual dose errors due to uncorrected liver rotation exist which may be corrected using different treatment adaptation strategies [10-12] to further improve the dosimetric accuracy.