Detailed analysis of patient stability during spine SBRT without immobilization
Isabel Remmerts de Vries,
The Netherlands
PO-1870
Abstract
Detailed analysis of patient stability during spine SBRT without immobilization
Authors: Isabel Remmerts de Vries1, Wilko Verbakel1, Max Dahele1, Ben Slotman1
1Amsterdam University Medical Center, Radiation Oncology, Amsterdam, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
Stereotactic body radiotherapy (SBRT) for treatment of spine metastases attempts to maximize target coverage and limit spinal cord/cauda equina dose through steep dose gradients. Accurate positioning and spine stability during treatment ensure consistency between planned and delivered dose. We analyzed our experience with online markerless 3D positional monitoring of the spine in patients undergoing spine SBRT without immobilization, on a TrueBeam platform.
Material and Methods
We have used non-clinical RapidTrack Realtime (RTR) software (Varian Medical Systems) to monitor spine position during stereotactic treatments. This analysis is concerned with patients treated using 5-fraction SBRT for lesions at thoracic vertebra 4 and lower, positioned using only a simple head rest with arm/knee supports. Prior to treatment, for each gantry angle, a digitally reconstructed radiograph, the template, is generated of the vertebra within the PTV. During 10MV FFF VMAT delivery, kV fluoroscopic images are continuously acquired (7/second) and online registered with the nearest template (on a separate computer with no control over the LINAC), resulting in 2D positions of the tumor. Each 2D registration is triangulated with multiple 2D positions from at least 14° earlier, resulting in a 3D target position. If RTR showed a deviation of >1mm in lateral, longitudinal or vertical direction, treatment was interrupted and a new CBCT-based couch correction was performed.
Results
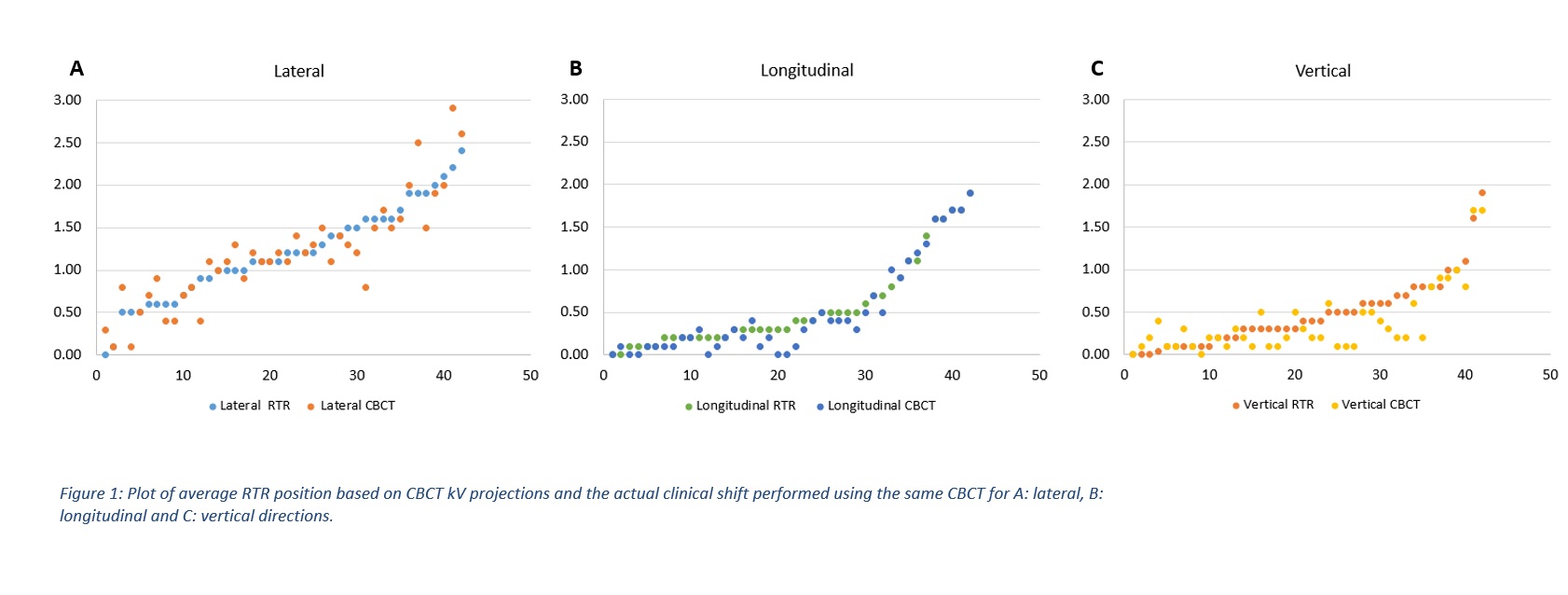
We analyzed 22 patients. Median age 62 years, 55% were male. Average time between start 1st imaging and end of 2nd (final) arc was 17.3 minutes (8.1-50.2). Figure 1 shows agreement in 3 translational directions between the mean RTR position derived from CBCT kV projections and the actual clinical shift performed using the same CBCT after treatment interruption. 97% of the data points agree to within 0.5mm and 90% within 0.3mm. Out of 220 arcs, MV delivery was interrupted 44 times (36/8 in 1st/2nd arcs respectively; average 35s after start of the arc; 25/44 for lateral deviation). 9 patients had ≥3 interventions and 8 no interventions. In 12/44 cases the CBCT after interruption showed translational shifts <1mm (mean 0.7mm, SD 0.2mm). 22 interruptions were during L-spine treatments (n=10) and 21 during T-spine (n=12). Absolute mean (SD) lateral/longitudinal/vertical CBCT-based shifts were 1.2(0.6)/0.5(0.5)/0.4(0.4)mm. Correlation coefficient between lateral CBCT shift and magnitude of earlier roll correction was 0.5.
Conclusion
RTR and CBCT determined positions agree well. RTR spine tracking can be used to trigger CBCT acquisition and patient re-positioning during spine SBRT. Most patients are very stable (within 1mm of intended position) for most of the time, despite no immobilization. Lateral movement is the most prominent and vigilance is required especially after prior roll correction and at the start of the arc.