Comparison of Diode Array, Radiochromic Film and OSL Film Dosimeters for Patient Specific QA
Laurence Delombaerde,
Belgium
PO-1777
Abstract
Comparison of Diode Array, Radiochromic Film and OSL Film Dosimeters for Patient Specific QA
Authors: Marco Caprioli1, Laurence Delombaerde2, Nicole De Keyzer3, Luana de Freitas Nascimento4, Robin De Roover5, Katleen Himschoot6, Brent van der Heyden4, Dirk Vandenbroucke6, Paul Leblans6, Wouter Crijns2
1KU Leuven, Laboratoty of Experimental Radiotherapy, Leuven, Belgium; 2UZ Leuven, Radiation Oncology, Leuven, Belgium; 3PTW Freiburg GmbH, PTW benelux, Freiburg, Germany; 4SCK CEN , Research in Dosimetric Application group, Mol, Belgium; 5UZ Leuven, Oncology Department, Leuven, Belgium; 6Agfa N.V., Corporate Innovation Office, Mortsel, Belgium
Show Affiliations
Hide Affiliations
Purpose or Objective
The present study evaluates the performance of three multidimensional dosimeters used for radiotherapy patient-specific QA (PSQA).
Material and Methods
10 clinical 6MV flattening filter free (FFF) SBRT plans (Table 1) were selected. The dose was calculated with the ACUROS algorithm (16.1.0) available on Eclipse (Varian Medical Systems). The plans were delivered on a TrueBeam STx linac. The Octavius® 1500 detector (O4D, from PTW) performed a real-time 3D dose integration using its rotational phantom. A longitudinal resolution (res) of 5mm was obtained merging two measurements with a 5mm gun-to-target couch shift. 10 GafchromicTM EBT3 films (Ashland) and an erasable optically stimulated luminescence (OSL) research film (QUARTEL project) were used in a Mcube phantom (IBA). The EBT3s were scanned 48h after the irradiation with a Flatbed CCD scanner (res 0,175mm) and converted to dose via a red channel optical density calibration on 2 additional calibration films as used in our local protocol. The luminescence was digitized with a CR scanner (res 0.1mm, AGFA) 10min after irradiation. After a flood field homogeneity correction on the raw image, the signal was linearly converted to dose with a calibration in the dose range 0.5-15Gy. The measured dose of the three detectors was rescaled using a factor (krescale) calculated as the median local dose difference within the 50% region from the DTPS,max. With DTPS,max as the reference, a 3%/2mm 3D global gamma was calculated with 50% low-dose threshold on the O4D (PTW, VeriSoft®). All 2D global gamma analysis (3%/2mm, 50% low-dose-threshold) were performed in a third party software (MyQA® patient, IBA) on the coronal dose plane measured at the isocenter with the three detectors.
Results
The krescale are listed in Table 1. The O4D has the lowest average rescaling and 1σ (1.035±0.019), suggesting a higher accuracy and precision. The EBT3s dose difference might be due to a calibration aging effect (under study). The OSL accuracy can improve with a calibration considering its signal fading and energy dependence. After the rescaling, with the exception of the SBRT sacral treatment, the O4D showed a 3D agreement score >97.5%. When used in a 2D dose plane projection the score is >91%. The mm-intracranial target volume requires a detector with a higher resolution. For EBT3s the 2D agreement score is 100% unless for the adrenal plan, which is 94.8%. The same trend was captured by the OSL film with an agreement score> 92%.
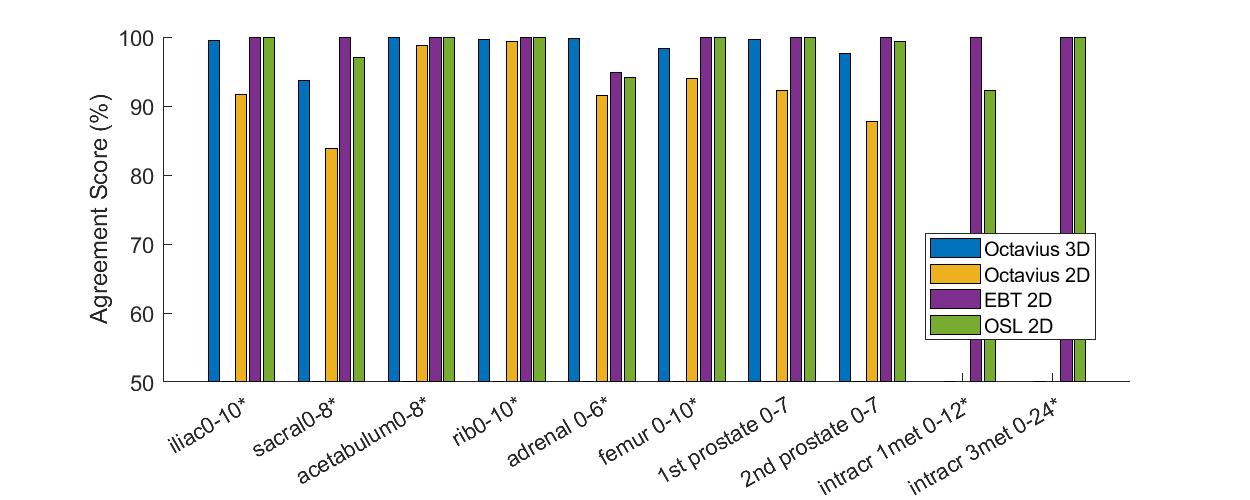
Fig.1: global gamma (3%/2mm, 50% low-dose-thresold) with DTPS,max as reference.
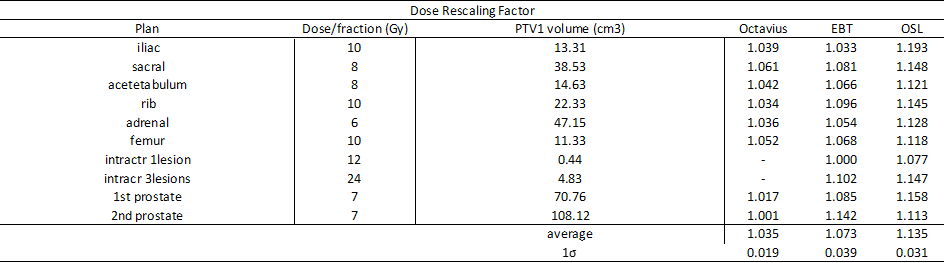
Tab.1: dose rescaling factors.
Conclusion
The O4D and OSL film allow fast-in-time acquisitions in contrast to EBT3 films. The O4D has the lowest krescale and 1σ and can be used for 3D dose measurement. On the other side, the OSL system has the highest resolution (0.1mm) followed by EBT3s (0.175mm) and can be used for mm-target s after the development of an accurate calibration. The three detectors, when used for high dose PSQA, showed an agreement score >91%.