Tumor control probability-based criteria for clinical trial credentialing
Vanessa Panettieri,
Australia
PO-1758
Abstract
Tumor control probability-based criteria for clinical trial credentialing
Authors: Vanessa Panettieri1, Paige Taylor2, Stephen F Kry2
1Alfred Health Radiation Oncology, Alfred Health , Melbourne, Australia; 2Imaging and Radiation Oncology Core, Department of Radiation Physics, MD Anderson Cancer Center, Houston, USA
Show Affiliations
Hide Affiliations
Purpose or Objective
Clinical trial credentialing in North America requires every institution to successfully irradiate an IMRT phantom (based on head and neck anatomy) from the Imaging and Radiation Oncology Core (IROC). Planned and measured doses must agree within 7% throughout the phantom. This criterion is based on dosimetric agreement and is uniformly applied to clinical trials for all anatomical sites. In this study we examined tumour control probability (TCP) as an alternate means to define credentialing criteria.
Material and Methods
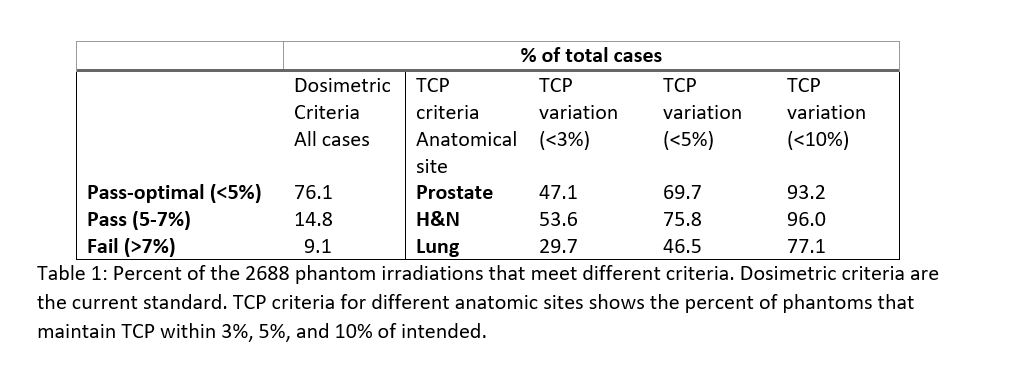
2688 irradiations of IROC’s IMRT (H&N) phantom were conducted between 2004 and 2022 by different radiotherapy centres. For each irradiation, absolute doses to 6 TLD, centrally located within the CTV, were measured. These 6 values were used to generate CTV differential DVHs (dDVH) relative to planned, and Tumour Control Probability (TCP) using the Marsden model [1] (BioSuite Vn 12.01). Three anatomical sites were studied: H&N, prostate and lung. TCP model parameters were derived from the literature, adjusting when required to fit clinical outcome data. Phantom dose deviations producing TCP variations of 3%, 5% and 10% were analysed and compared to the established dosimetric criteria: pass-optimal (95%-105% maximum dose disagreement between planned and measured), pass (93-95% and 105-107%) and fail (< 93%, >107%).
when required to fit clinical outcome data. Phantom dose deviations producing TCP variations of 3%, 5% and 10% were analysed and compared to the established dosimetric criteria: pass-optimal (95%-105% maximum dose disagreement between planned and measured), pass (93-95% and 105-107%) and fail (< 93%, >107%).
Results
Using current dosimetric criteria 2046, 397 and 245 phantoms were scored as pass-optimal (<5%), pass (5-7%) and fail (>7%); Table 1. When these results were re-sorted based on TCP criteria, the percent of acceptable results depended strongly on anatomical site; 54% of phantom irradiations maintained a H&N TCP within 3%, but only 30% maintained a lung TCP within 3%. The lung, in particular, showed poor consistency in TCP: 23% of phantom irradiations failed to maintain a TCP within 10%.
There was reasonable but not perfect alignment between dosimetric and TCP-based criteria. For example, to maintain a 10% TCP for the prostate, a dosimetric criteria of 7% produces similar results. However, there is not perfect agreement; for example there are many individual cases where the irradiation result passes the 7% dosimetric criterion but falls outside of the 10% TCP criterion. Such cases emphasize that the current dosimetric criterion does not always capture the full biological impact of deviations in the credentialing phantom.
Conclusion
TCP-based criteria provide a novel lens for clinical trial credentialing. Such an approach could tie better into the needs of clinical trials by providing outcome-based criteria as well as incorporating the different sensitivity of different anatomic sites. This approach also reinforced that current dosimetric criteria for clinical trial credentialing are likely too loose, particularly for dosimetrically sensitive sites such as the lung, and dosimetric criteria may not fully capture the impact on outcome.