Sensitivity of myQA SRS detector to intentional errors in HyperArc plans.
PO-1755
Abstract
Sensitivity of myQA SRS detector to intentional errors in HyperArc plans.
Authors: Nina Cavalli1, Elisa Bonanno1, Giuseppina Borzì1, Alessia D'Anna2, Martina Pace1, Giuseppe Stella3, Lucia Zirone1, Carmelo Marino1
1Humanitas-Istituto Clinico Catanese, Medical Physics Department, Misterbianco (CT), Italy; 2University of Catania, Physics and Astronomy E. Majorana , Catania, Italy; 3University of Catania, Physics and Astronomy E. Majorana, Catania, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
After a preliminary step of validation of IBA myQA SRS high resolution solid-state detector, we perform an evaluation in the context of the Stereotactic Radiosurgery (SRS) HyperArc (HA) treatments.
In this study, we check the ability of the myQA system to detect intentional errors related to the High Definition (HD) MLC position.
Material and Methods
Ten original SRS HA treatment plans (21Gy/1fx) and 30 plans with introduced delivery errors, for a total of 40 plans, were investigated. From the original plans, new plans with introduced errors of different magnitudes regarding the MLC were generated, using an “home-made” script. For each plan, MLC positioning errors were introduced, including widening of entire leaf bank A of 0.5 mm, 0.8 mm and 1 mm, respectively.
All plans were calculated on a TrueBeam machine equipped by HD MLC, using AcurosXB v.16.1 algorithm. Plans were delivered across myQA SRS detector, located inside myQA SRS phantom. The measurement sensors of myQA SRS are monolithic solid-state semiconductor sensors arranged in a 2D array and the detector is optimized to measure 2D dose maps of small fields with high resolution. The sensor layout is a grid of 300 x 350 pixels spaced of 400 µm in an area of 120 mm x 140 mm (active area).
The impact of the errors in the modified plans was assessed using myQA system’s inherent gamma analysis with local 2%/2mm and local 2%/1mm (with 5% threshold dose) criteria.
To assess the myQA systems’ability to detect introduced errors, we evaluated the gamma passing rate between the original and modified measured dose distribution for each plan. Gamma analysis was performed for each single arc of plans and for the integrated total dose distribution of plans.
Results
Tab. I shows, for brevity, results in terms of gamma passing rate for the integrated total dose distribution of plans. Employing local gamma analysis with 2%-2mm criteria, a substantial gamma pass rate difference is evident for only one case concerning the MLC error positioning of 0.8 mm (total gamma pass rate: 91.9%); while for the error of 1 mm, the gamma pass rate decrease is observed for two plans (total gamma pass rate:86-95.4%).
Using the more restrictive local gamma analysis with 2%/1mm, MLC error positioning of 1 mm was detected for all plans (total gamma pass rate: 68.7-95.1%); the 0.8 mm error was detected for 7 plans (total gamma pass rate: 72-94.9%); the 0.5 mm error was detected for two plans (total gamma pass rate: 82.2-95.0%).
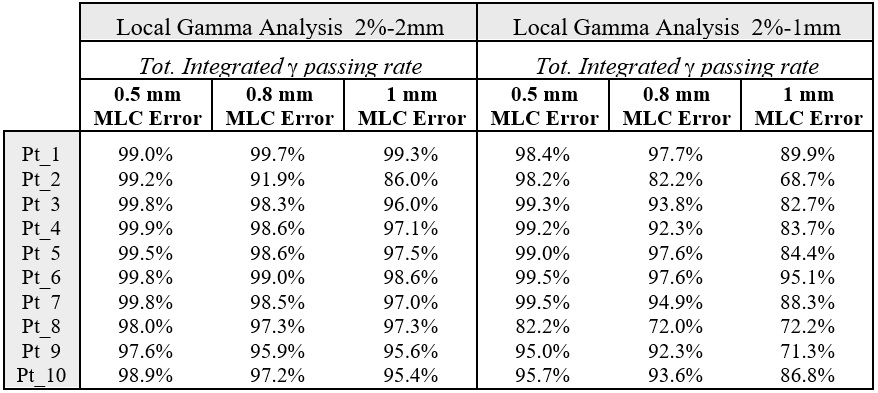
Tab. I Gamma pass rate (%) between original and modified measured distribution dose, for each patient(Pt) and for each magnitude of introduced error.
Conclusion
myQA system seems to be a valid tool to detect MLC positioning errors for SRS HA treatments. Using the 2%-1mm gamma evaluation criteria, the system has been able to detect MLC bank offsets of 1 mm for all studied plans and, for 7/10 plans, the MLC error of 0.8mm.
These results give confidence about the high accuracy of myQA system to detect relevant clinical errors for HA SRS treatments.