Challenges of online adaptive treatments verification
PO-1746
Abstract
Challenges of online adaptive treatments verification
Authors: Adam Galdi1, Szilvia Gazdag-Hegyesi1, Csilla Pesznyák1, Tibor Major1
1National Institute of Oncology, Radiotherapy, Budapest, Hungary
Show Affiliations
Hide Affiliations
Purpose or Objective
The on couch online adaptive radiotherapy is the most advanced radiotherapy approaches and it can be performed by a dedicated linear accelerator, called Ethos, from Varian. The aim of my project was to develop an online adaptation workflow verification and make point dose measurements with a commercial, non-dedicated tissue equivalent phantom.
Material and Methods
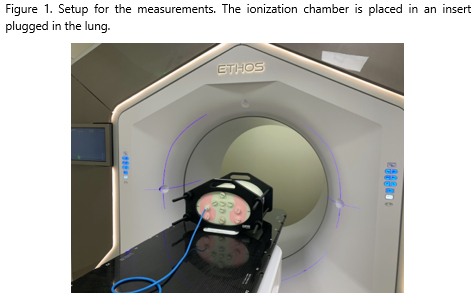
CIRS THORAX Phantom is available at our institute. The phantom accommodates soft, lung and bone tissue inserts in various positions with or without hole in the inserts (Figure 1.). A non-reference phantom set up was used because a soft tissue insert was plugged in the lung volume representing a lung tumour. A base line planning CT (pCT) was used for adapted planning in the Ethos. In the first step we evaluated the workflow, how the phantom and the set up could be used for online adaptation from the first CBCT followed by re-contouring/re-planning and to deliver the treatment fields with changing the position of the insert. Furthermore, the point doses were measured in “tumour” in different positions, selecting both adapted and scheduled plans. The positions of the soft tissue insert were changed representing the changes of tumour position. Original tumour position on pCT was in right lower “lobe”. Measurements were performed in three points. The first was the original position where the adapted and scheduled plan, and soft and lung tissue were used. Second position was the right upper “lobe” where the adapted and scheduled plan and soft tissue were used. Third position was the left upper “lobe”, where the soft tissue insert and the adapted plan was used only.
The accuracy of the image guidance was evaluated in the adaptation workflow with a pre CBCT before the treatment, with a manually shift of the phantom, simulating an inter-adaptation motion error. With these motions and re positioning the dose was measured.
Results
This non-dedicated phantom was used perfectly for the whole adaptation process, and we could simulate the change of tumour position and practise the adaptation without patient.
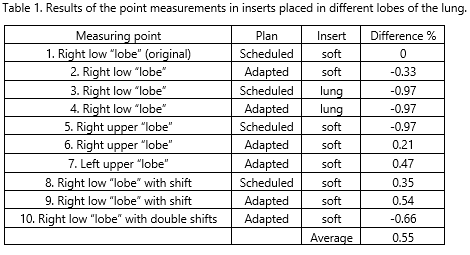
Comparing the point dose measurement of the base line situations with the adapted insert positions, the same dose was measured within ±0.55% (-0.97-0.54) regardless of whether the adapted or scheduled plan was chosen or the phantom was manually shifted (Table 1). In cases of worst-case scenarios of “tumour” change, where the soft tissue insert was in the left upper lobe, the scheduled plan was not optional. By evaluationing the heterogeneity corrections during adaptation, the same dose was measured in the soft tissue insert as in the lung tissue insert.
Conclusion
In our study, we demonstrated that a commercially available non-dedicated phantom can be used to exercise the whole adaptation workflow.
We proved with point measurements that the adaptations are safe regarding the tumour dose.
By evaluating the image guidance accuracy, precise dose delivery can be proved if inter-adaptation motion error is discovered before the treatment.