Evaluation of treatment delivery quality for right breast tomotherapy in prone position
Maud Jaccard,
Switzerland
PO-2032
Abstract
Evaluation of treatment delivery quality for right breast tomotherapy in prone position
Authors: Maud Jaccard1, Marie Fargier-Voiron1, Nicolas Perichon1, Cédric De Marco1, Oscar Matzinger1, Shelley Bulling1, Francesca Caparrotti2
1Swiss Medical Network, Radiation Oncology, Geneva, Switzerland; 2Swiss Medical Network, Radiation Onoclogy, Geneva, Switzerland
Show Affiliations
Hide Affiliations
Purpose or Objective
To report our initial experience for right breast radiotherapy in prone position and to evaluate the dosimetric impact of residual setup errors for tomotherapy treatment delivery.
Material and Methods
Three right breast patients were scanned in supine and prone position. Targets and OARs were delineated on both scans. Radiotherapy consisted of 50 Gy in 25 fractions to the whole breast, with a simultaneous boost to the tumor bed of 60 Gy. Treatment plans were prepared in RayStation 11A using a TomoHelical technique for supine and TomoDirect technique for prone position. We used the robustness function in RayStation to create an additional 1-cm leaf opening around the breast for both techniques. The radiation oncologist selected the best plan for treatment. Initial setup was performed using an optical surface monitoring system and skin marks on the right breast. Treatment was delivered on a Radixact equipped with kVCT for pre-treatment imaging verification. A second kVCT was acquired at the end of the first fraction to evaluate intrafraction motion. Dose was computed on the 25 daily pre-treatment kVCTs using the online registration from the treatment session, and deformed target and OAR volumes (checked and corrected by the radiation oncologist). The daily dose distributions were compared to the reference plan using dose volume parameters. In addition, each fraction dose was deformed back on the planning CT, and the accumulated summed dose was compared to the reference plan.
Results
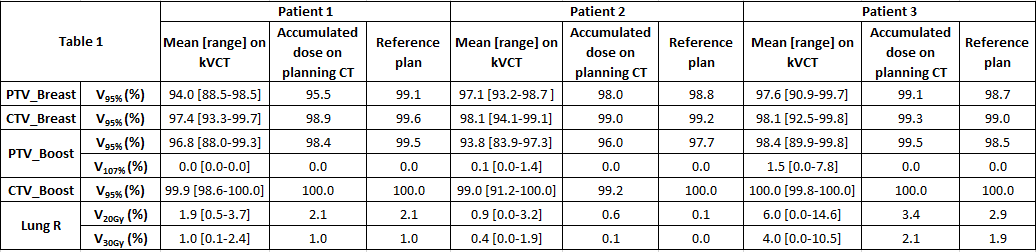
Three prone TomoDirect plans were selected for treatment. For similar target coverage, dosimetric results were significantly better in prone position, with reduction in heart (0.5-prone vs. 2.2 Gy-supine), LADA (0.4 vs. 1.6 Gy), right lung (3.1 vs. 8.1 Gy) and left breast (0.5 vs. 1.5 Gy) mean doses for all patients. Median setup time (defined as the time between patient entering the treatment room and beam start) was 6.5 min (range 4.8-13.9 min). End of session kVCTs showed no clinically relevant shifts compared to the pre-treatment kVCT. Radiotherapy was delivered with 5 or 6 TomoDirect beams with total beam-on times ranging from 187 to 220 s. Dose calculations on pre-treatment images showed that the mean PTV V95% could be reduced below 95%, but that mean CTV V95% was always above 97% (Table 1), both for the boost and the whole breast PTV. The PTV V107% remained below 2%. Accumulated dose on the planning CT resulted in excellent dosimetric parameters for the CTVs and PTVs, and sparing of the right lung similar to the reference plan.
Conclusion
Our results indicate a significant clinical advantage of prone right breast tomotherapy compared to the supine position, with improved OAR sparing. Using robust planning in RayStation, and optical surface monitoring and kVCT for setup, allows for optimal positioning and adequate dose delivery to the targets. Further investigation is needed in order to confirm our findings on a larger patient cohort.