Real-world electronic patient reported outcome utilization in patients receiving radiation therapy
PO-1593
Abstract
Real-world electronic patient reported outcome utilization in patients receiving radiation therapy
Authors: Ian Kudel1, Heather Curry1, Paula Pennanen2, Mari Lahelma3, Joni Vuorio2, Riikka-Leena Leskelä2, Zoya Shamsi1, Maarit Bärlund4
1Varian, a Siemens Healthineers Company, Global Evidence and Value, Palo Alto, USA; 2Nordic Healthcare Group, NHG Finland, Advisory Business Unit, Helsincki, Finland; 3Nordic Healthcare Group, NHG Finland, Advisory Business Unit, Helsinki, Finland; 4Tampere University Hospital and University of Tampere, Department of Oncology, Tays Cancer Center, and Faculty of Medicine and Health Technology, Tampere, Finland
Show Affiliations
Hide Affiliations
Purpose or Objective
Prospective randomized trials have demonstrated that ePRO usage can improve outcomes for those receiving systemic therapy, but few data exist regarding its utilization in patients receiving radiation therapy (RT) as part of their care. The aim of this study is to better understand the experiences of these patients
Material and Methods
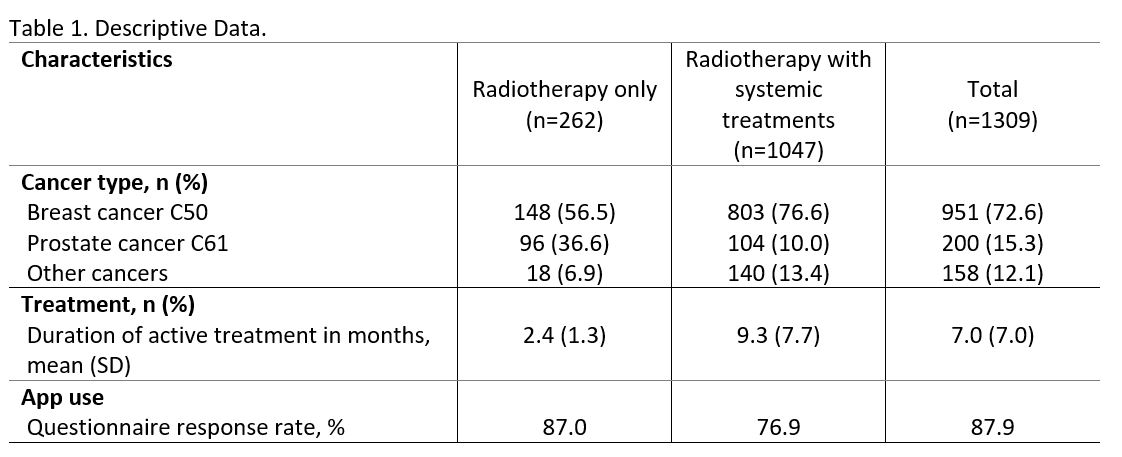
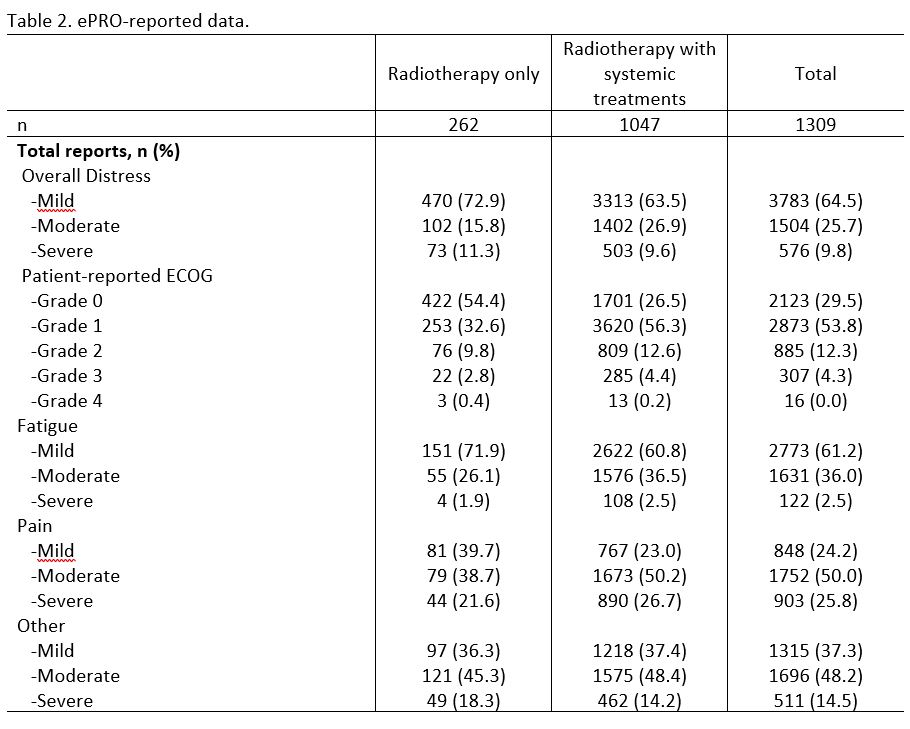
Participants (n=1309) were Tampere University Hospital cancer patients that received radiotherapy (RT) or RT + systemic treatment between 2015 and 2021 and also used the app to respond to symptom module questionnaires. All symptom modules ask patients to report their overall distress via an 11-point scale (0=none,10=Worst Possible) and functioning using an ECOG-based item. Additionally, patients can report treatment-related symptoms using a Common Terminology Criteria for Adverse Events (v5) response framework. The CCT administers the questionnaire on a regular cadence throughout active treatment. When a patient reports moderate or severe symptoms a real-time electronic alert is generated which prompts the CCT to offer clinical recommendations via the app. Patients’ electronic health record data along with ePRO usage were matched and analyzed descriptively
Results
Participants were predominantly female (n=1026,78.4%) and middle-aged (M=63.0,SD=11.3). The majority of patients had a primary diagnosis of either breast (72.6%) or prostate cancer (15.3%). Most received standard-of-care RT + some form of systemic therapy (n=1047;80%;Table 1) and were in active treatment longer. The mean number of questionnaires administered was 10.0 (SD=12.9) and the overall response rate of 87.9%. Table 2 indicates that RT patients generally reported low distress and adequate performance status (patient-reported ECOG performance status grade of 0 or 1; Table 2), but it should be noted that 27.1% of patients reported moderate-to-severe distress at least one time. The three RT treatment symptoms that patients reported the highest levels of moderate-to-severe symptomatology, at least one time, were “other” (64.6%), pain (60.3%), and fatigue (28.0%). Patients receiving RT + systemic therapy reported, comparatively, higher levels of distress, worse physical performance, and higher reports of moderate and severe pain (76.7%), “other” (62.6%), and fatigue (39.0%).
Conclusion
Despite varying regimens and treatment schedules (daily RT lasting several weeks to monthly systemic treatments) patients consistently used an ePRO to report their experiences. This systematic method of quantifying the patient voice compliments standard-of-care treatment by hastening the recognition of patient distress regardless of treatment modality and facilitates continuity of care. Finally, the ePROs wide, sustained use is a behavioral indicator that patients value its use during a vulnerable period in their cancer journey.