Moderately hypofractionated proton therapy with implantable spacer in patients with prostate cancer
Vicky Kaviraj Soborun,
Germany
PO-1482
Abstract
Moderately hypofractionated proton therapy with implantable spacer in patients with prostate cancer
Authors: Vicky Kaviraj Soborun1, Angelika Borkowetz2, Julia Thiele1, Steffen Löck3, Christian Thomas2, Esther G. C. Troost1, Mechthild Krause1, Tobias Hölscher1
1Faculty of Medicine and University Hospital Carl Gustav Carus, Technische Universität Dresden, Department of Radiotherapy and Radiation Oncology, Dresden, Germany; 2Faculty of Medicine and University Hospital Carl Gustav Carus, Technische Universität Dresden, Department of Urology, Dresden, Germany; 3OncoRay – National Center for Radiation Research in Oncology, Faculty of Medicine and University Hospital Carl Gustav Carus, Technische Universität Dresden, Helmholtz-Zentrum Dresden - Rossendorf, Dresden, Germany
Show Affiliations
Hide Affiliations
Purpose or Objective
Hypofractionated radiotherapy is becoming popular in the treatment of localized prostate cancer, even though the rectum remains a dose-limiting structure. The use of an implantable retroprostatic spacer [(RPS), Prospace Ballon, Bioprotect Ltd, Israel] for the reduction of rectal toxicity has not been extensively studied for moderately hypofractionated proton beam therapy (PBT). This study therefore aimed to assess the gastrointestinal (GI) and genitourinary (GU) toxicities in patients with localized prostate cancer treated with moderately hypofractionated PBT and an implantable RPS, and to compare those to two schedules without RPS.
Material and Methods
In a single-institution retrospective analysis of prospectively collected data, three cohorts of patients with localized prostate cancer, irradiated between January 2015 and October 2020 were included: Arm 1 PBT up to 60 Gy(RBE) in 20 fractions [PBT with RPS], Arm 2 normofractionated 74-76 Gy(RBE) without RPS [PBT without RPS], and Arm 3 intensity modulated photon radiation therapy (IMRT) up to 60 Gy in 20 fractions without RPS [IMRT without RPS]. Patients’ characteristics as well as baseline complaints, early (at 3 months) and late toxicity (at 1 year) were compared using Pearson's chi-squared test. The level of significance was set at p < 0.05.
Results
From 101 patients identified, 33 men were grouped in Arm 1, 31 in Arm 2, and 37 in Arm 3. Three patients were dropped out from Arm 1 due to incomplete follow-up. Treatment was completed as planned in all patients. Baseline characteristics were well balanced except for prostate volume (p=0.009, lower volume in Arm 1, see Table 1). Baseline symptoms as well as acute GI and GU toxicity were comparable between Arm 1 and Arm 2. Late GU toxicity was significantly higher in Arm 1 compared to Arm 2 (Grade ≥1: 70% vs 54.8%, p=0.015). Late grade ≥2 GI toxicity was significantly more frequent in men who received PBT without the RPS (13% vs 0%, for Arm 2 vs 1, respectively, p=0.042). When comparing Arm 1 to Arm 3, we found no statistically significant differences, neither in baseline nor in early GI/GU toxicity. Assessment of late toxicity in this case was incomplete.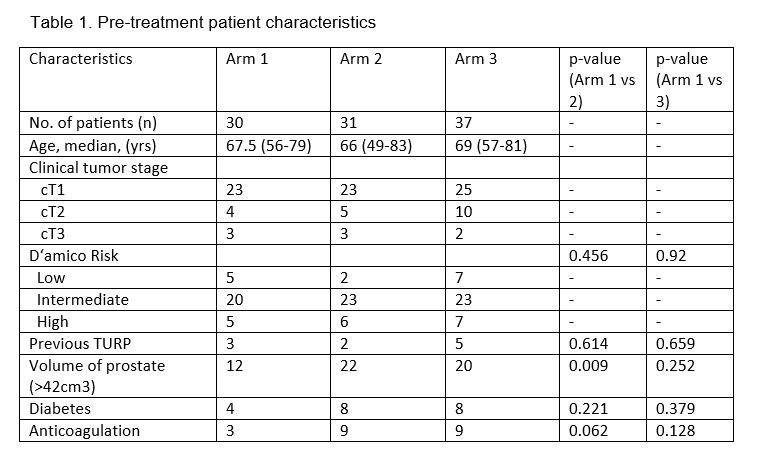
Conclusion
Our study demonstrated that an implantable spacer helps in reducing grade > 2 GI toxicity in patients receiving PBT. However, further evaluation and follow-up is needed to assess if there is a same benefit of PBT with RPS when compared to IMRT without RPS.