PSMA-guided management of oligorecurrent post-prostatectomy patients: focus on SBRT
Giuseppe Carlo Iorio,
Italy
PO-1456
Abstract
PSMA-guided management of oligorecurrent post-prostatectomy patients: focus on SBRT
Authors: Giuseppe Carlo Iorio1, Erica Maria Cuffini1, Valeria Chiofalo1, Cristiano Grossi1, Sara Bartoncini1, Veronica Richetto2, Ilaria Bonavero1, Diego Bongiovanni1, Giuliana Petruzzellis1, Mario Levis1, Guido Rovera3, Serena Grimaldi3, Beatrice Lillaz4, Marco Oderda4, Paolo Gontero4, Désirée Deandreis3, Umberto Ricardi1
1University of Turin, Department of Oncology, Turin, Italy; 2University of Turin, Department of Medical Physics, Turin, Italy; 3University of Turin, Department of Medical Sciences, Nuclear Medicine, Turin, Italy; 4University of Turin, Department of Surgical Sciences, Urology, Turin, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
To evaluate the impact of PSMA-PET in the management of oligorecurrent post-prostatectomy (RP, +/- prostate bed RT) prostate cancer (PCa) patients, with a focus on metastasis-directed therapy (MDT),namely SBRT.
Material and Methods
This analysis is part of a prospective, open label, observational, single-centre study testing the PSMA-PET performance in recurrent hormone-sensitive PCa patients. Patients with biochemical recurrence (BCR, PSA>0.2 ng/ml) following RP +/- prior prostate bed RT (PB-RT, adjuvant-ART or salvage-SRT) were staged with PSMA-PET. This analysis pertains to PSMA-positive patients only. The primary endpoint was to assess the biochemical progression-free survival (bPFS) resulting from the therapeutic approaches employed for the different recurrent sites; patients with an exclusive PB-recurrence and no prior PB-RT were excluded from the analysis. The ADT-free interval was evaluated in patients treated with exclusive SBRT.
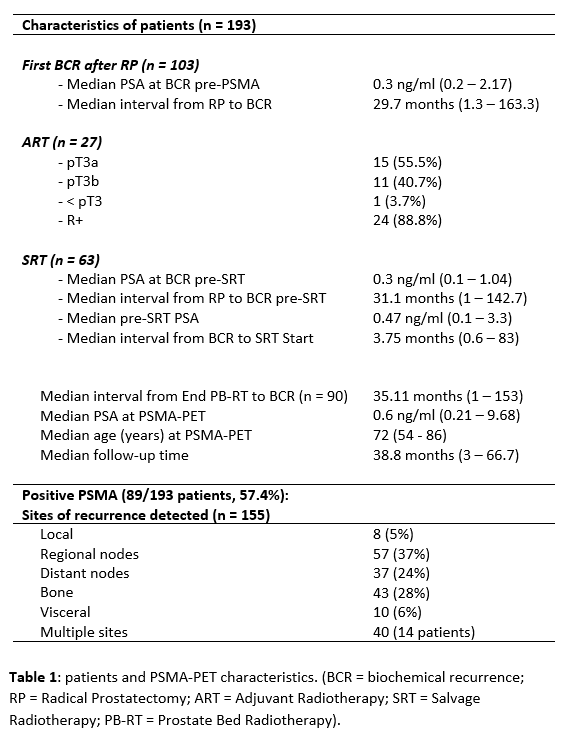
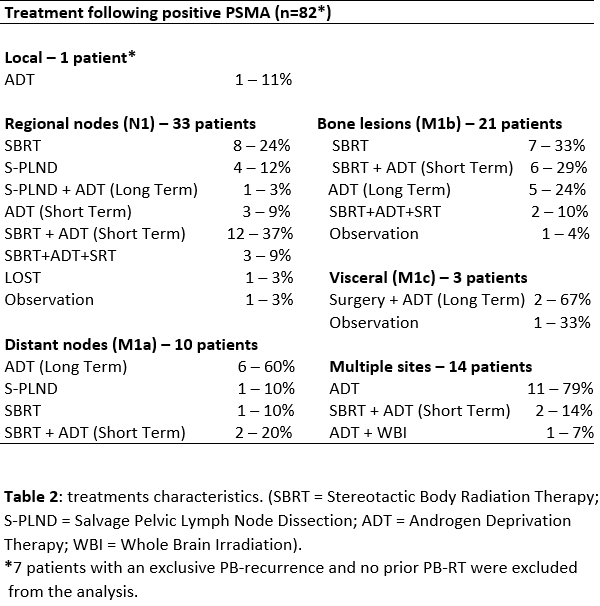
Results
Data from 193 patients staged with PSMA-PET (June 2016-April 2022) for BCR after RP (pN0-pNx) were prospectively collected. Median follow-up was 38.8 months (mos). 89/193 PSMA-positive patients (46.11%) were included in the present analysis, with 155 lesions detected. 7 patients with an exclusive PB-recurrence and no prior PB-RT were excluded from the analysis. The most common failure site was N1, with 57 lesions detected in 33 patients (37%); 10 patients (11.3%) had M1a, 21 (23.6%) had M1b, 3 patients (3.4%) had M1c, while 14 patients (15.7%) had multiple lesions. Tables 1-2 show patient, PSMA and treatment details. Hereby, we report mainly the MDT cohorts outcomes per recurrent site. In 22/89 cases (24.7%) SBRT + ADT was administered: 13 N1, 2 M1a, 6 M1b, 1 N1+M1b. The median bPFS of this cluster was 9.9 mos (range 3 – 39.5), and 12/22 patients recurred after median interval of 9.5 mos. Exclusive SBRT was administered in 16/89 patients (17.9%): 8 N1, 1 M1a, 7 M1b. The median bPFS was 8.3 mos (range 3.5 - 42), with 13/16 patients recurring after a median interval of 7.8 mos (range 3.5 – 30). After a median interval of 19.5 mos, 6/13 patients underwent a second SBRT round (+ADT in 3/6 patients) achieving a median bPFS of 8.3 mos (1 – 23.3). 1/13 patients underwent exclusive ADT. An observational approach was adopted in 6/13 cases, contributing to an overall median ADT-free interval of 31.2 mos. 5/89 patients (5.6%) underwent salvage surgery (4 N1, 1 M1a) with a median bPFS of 6.6 mos (range 1 – 11.7). 26/89 patients underwent exclusive ADT following positive PSMA findings, and at the present analysis only 2 developed castration-resistance.
Conclusion
PSMA-PET allows treatment tailoring for oligorecurrent hormone-sensitive PCa patients, particularly MDT. Exclusive SBRT can delay ADT-initiation, and multiple SBRT rounds should be evaluated in selected patients. The optimal approach in this oncologic scenario remains to be defined. Along with modern molecular imaging, genetic predictors are set to recover a major role in treatment guidance.