Health-related quality of life in extreme hypofractionation for localized prostate cancer
PO-1493
Abstract
Health-related quality of life in extreme hypofractionation for localized prostate cancer
Authors: Ilaria Bonavero1, Giuseppe Carlo Iorio1, Giuliana Petruzzellis1, Diego Bongiovanni1, Sara Bartoncini1, Elena Gallio2, Valeria Chiofalo1, Erica Maria Cuffini1, Cristiano Grossi1, Mario Levis1, Umberto Ricardi1
1University of Turin, Department of Oncology, Turin, Italy; 2University of Turin, Department of Medical Physics, Turin, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
Extreme hypofractionation is gradually becoming a mainstay of treatment for prostate cancer (PCa). Patients’ (pts) tolerance to such RT regimes is certainly under the spotlight. Herein, we report health-related quality of life (HRQOL) data in a single-center observational study.
Material and Methods
In this observational study of a consecutive series of low- to high-risk PCa pts treated with (LINAC-based VMAT) extreme hypofractionation (42.7 Gy/7 fractions) +/- ADT, HRQOL up to 1 year from treatment was evaluated through the italian short-form of the UCLA-Prostate Cancer Index (-PCI). This short-form is a self-administered 14-item questionnaire that quantifies prostate-specific HRQOL in six domains, urinary function (UF) and bother (UB), bowel function (BF) and bother (BB), and sexual function (SF) and bother (SB). The scales are scored from 0 to 100, with higher scores representing better health states. The questionnaire was administered at baseline, RT end, 1-month (mo), 3-mos, 6-mos and 12-mos from the end of RT. Moreover, IPSS scores and RTOG toxicity were simultaneously recorded to address a complete tolerance evaluation.
Results
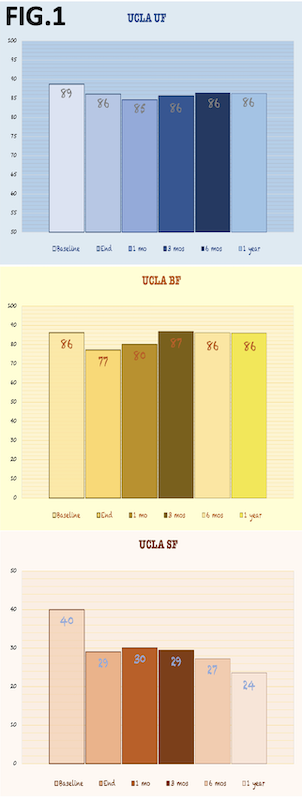
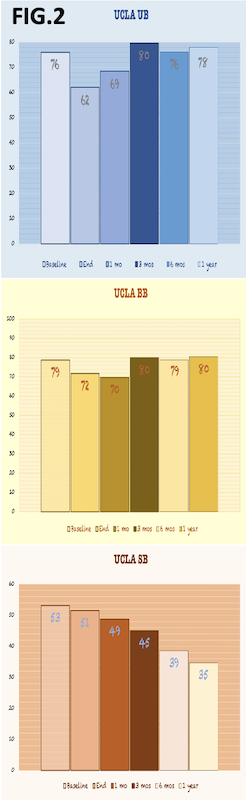
117 pts (mean age 74 years) were treated between May 2020 and September 2021. At RT end 70% of pts were undergoing ADT, 53% at 3-mos, 28% at 6-mos, only 24% at 1-year. An IPSS score >12 at the baseline was reported for the 21.4% of the population. UF did not significantly change along the timepoints, with mean scores ranging from 89 at baseline to 86 at 1-year (Fig. 1). UB dropped significantly at RT end (mean score 62 vs 76 at baseline), and gradually improved with equivalent/slightly higher scores than baseline from 3-mos to 1-year (Fig. 2). This in line with: RTOG GU G2+ toxicity, which peaked at RT end (20.5%) and gradually decreased at 3-mos (0%) with negligible rates at 1-year (3.4%); and with mean IPSS scores, that peaked at RT end (13 vs 8.4 baseline) and gradually decreased at 3-mos (8.6) and 1-year (7.7). BF dropped at RT end (mean score 77 vs 86 at baseline), and gradually improved with equivalent/slightly higher scores than baseline from 3-mos to 1-year (Fig. 1). BB dropped at 1-mo (mean score 70 vs 79 at baseline), and gradually improved with equivalent/slightly higher scores than baseline from 3-mos to 1-year (Fig. 2). In this regard, RTOG GI G2+ rates were overall negligible: 1.7% at RT end, and 0.8% at 3-mos and 1-year.SF and SB (Fig. 1-2) gradually decreased along the timepoints, with the mean lowest scores recorded at 1-year: 24 for SF (vs 40 at baseline) and 35 for SB (vs 53 at baseline).
Conclusion
In line with the RTOG GU toxicity assessment and the IPSS scores’ trend, UB improved over time following extreme hypofractionation, with a satisfactory regain at 1 year of the baseline condition. UF remained substantially stable, according to the patient’s reports. Bowel HRQOL appeared not to be severely impacted. The low baseline and overall scores for both SF and SB were in line with the mean age of the population and the ADT use.