Radiation therapy in patients with non-small cell lung cancer and interstitial lung abnormalities
PO-1340
Abstract
Radiation therapy in patients with non-small cell lung cancer and interstitial lung abnormalities
Authors: Makoto Ito1, Takuma Katano2, Hiroaki Okada1, Ami Sakuragi3, Yoshitaka Minami3, Souichiro Abe1, Sou Adachi1, Yukihiko Oshima1, Akihito Kubo2, Takayuki Fukui4, Satoru Ito2, Kojiro Suzuki1
1Aichi Medical University Hospital, Department of Radiology, Nagakute, Japan; 2Aichi Medical University Hospital, Department of Respiratory Medicine and Allergology, Nagakute, Japan; 3Aichi Medical University Hospital, Department of Central Radiology, Nagakute, Japan; 4Aichi Medical University Hospital, Division of Chest Surgery, Department of Surgery, Nagakute, Japan
Show Affiliations
Hide Affiliations
Purpose or Objective
To investigate the influence of radiotherapy for lung cancer on interstitial lung abnormalities (ILA).
Material and Methods
We retrospectively analyzed patients with non-small cell lung cancer who were treated with radiotherapy intended for radical or salvage for recurrence from 2010 to 2021. The standard dose fractionation was 60 Gy in 30 fractions. We divided the patients into three groups: normal (NL), ILA, and interstitial lung disease (ILD). In accordance with prior research, the term ILA was defined as specific CT findings that are potentially compatible with ILD in patients without clinical indication of the disease. ILA patients were further subdivided into non-subpleural (NS), subpleural non-fibrotic (SNF), and subpleural fibrotic (SF) groups. The grouping was performed independently by a chest physician and a diagnostic radiologist; the discrepant cases were confirmed upon consultation with another radiologist. The analysis of survival was performed on cases for radical intent.
Results
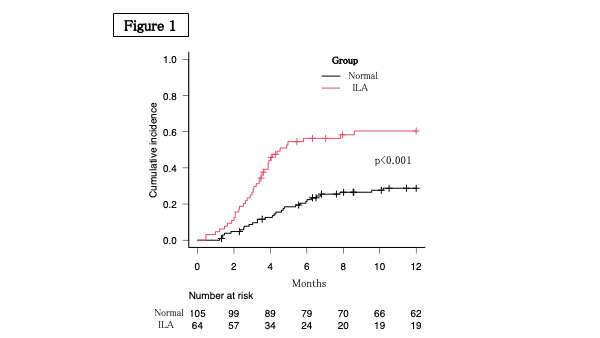
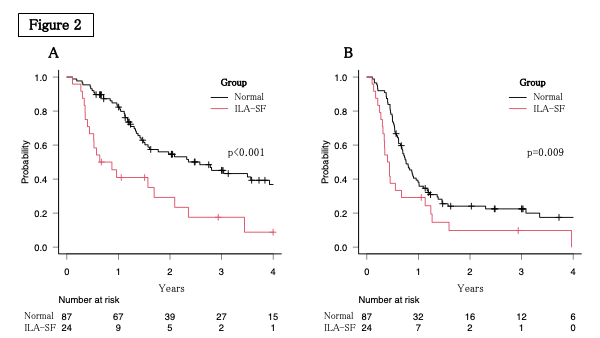
The number of patients was 175 (NL=105, ILA-NS=5, ILA-SNF=28, ILA-SF=31, ILD=6), and the median follow-up period for survivors was 2.5 years. Grade ≥ 2 radiation pneumonitis (RP) was observed in 71 patients (41%). The cumulative incidence of RP was higher in the ILA group compared to the NL group (p<0.001, Figure 1) in univariate analysis. In addition to the ILA group, {HR=2.4(1.3-4.7), p=0.008}, V10 (p=0.03) and V20 (p=0.01) of the lung contributed to RP in multivariate analysis. Grade 5 RP was observed in 8 patients (5%), in the ILA group (SF=7, SNF=1). The 2-year survival (overall survival, OS and progression-free survival, PFS) after radical irradiation was as follows: (48%, 21%) of the total 134, (55%, 24%) in the 87 NL group, (35%, 17%) in the 43 ILA group, and (29%, 10%) in the 24 ILA-SF group. The grouped OS is shown in Figure 2A and the PFS in Figure 2B. Multivariate analysis showed no difference between the NL group and the ILA group; however, both, OS (p=0.007) and PFS (p=0.03) were significantly shorter in the ILA-SF group compared to the NL group. Further, adenocarcinoma and durvalumab were independent contributors to OS and PFS prolongation.
Conclusion
ILA may be an important risk factor for RP. RP can have severe manifestations, especially in patients with ILA-SF and influence prognosis. Therefore, these findings are important in decision-making prior to radiation therapy.