Breath hold for photon or proton therapy in radical radiotherapy for lung cancer: worth the effort?
Judith van der Stoep,
The Netherlands
PO-1334
Abstract
Breath hold for photon or proton therapy in radical radiotherapy for lung cancer: worth the effort?
Authors: Esther Kneepkens1, Judith van der Stoep1, Anouk Vullings1, Janou Buck1, Marije Velders1, Michel Öllers1, Lieke in 't Ven1, Judith van Loon1, Dirk de Ruysscher1, Stephanie Peeters1
1Maastricht University Medical Centre+, Department of Radiation Oncology (MAASTRO), GROW School of Oncology, Maastricht, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
Reducing breathing motion through inspirational breath hold (IBH) could benefit both proton and photon therapy of lung tumors, as it allows for margin reduction and leads to a larger lung volume compared to free breathing (FB) treatments. For protons, IBH would also mitigate the interplay effect. In this study, we compared proton and photon FB and IBH plans in terms of their dosimetric differences and normal tissue complication probability (NTCP).
Material and Methods
Nineteen patients with locally advanced stage III or oligometastatic NSCLC, treated with radical RT were included. Four treatment plans, with a prescribed dose of 30 x 2 Gy, were compared: photon and proton plans, on both a FB 4DCT scan and an IBH scan.
For the photon FB plans, individual CTV-PTV margins were calculated for the CTV of the primary tumor (CTVp) [1]. For the IBH plans, this PTV-margin was 8mm. A 5mm margin was used for nodes (CTVn) in both plans. For the proton plans, a 3mm margin around CTVp and 0mm around CTVn were added for a GTV-amplitude on 4DCT <5mm, or an ITV was created with extra 2mm margin for >5mm; both combined with 3D robust optimization with an isotropic setup shift of 5mm and 3% density uncertainty.
VMAT photon therapy plans were made for a Truebeam STx using 2 half-arcs. IMPT plans were made for a Mevion S250i Hyperscan system with 2-3 beam directions. The same beam arrangement was used for IBH and FB plans. Differences in doses to OAR and relevant NTCPs were evaluated [2-4].
Results
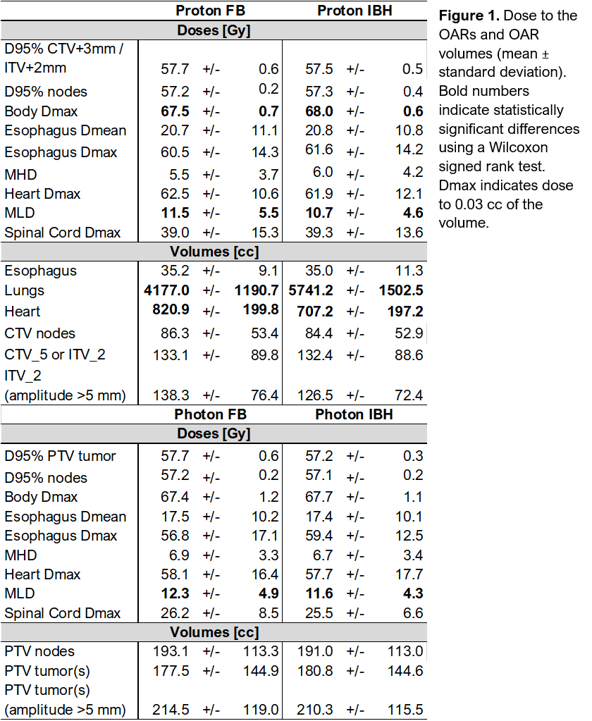
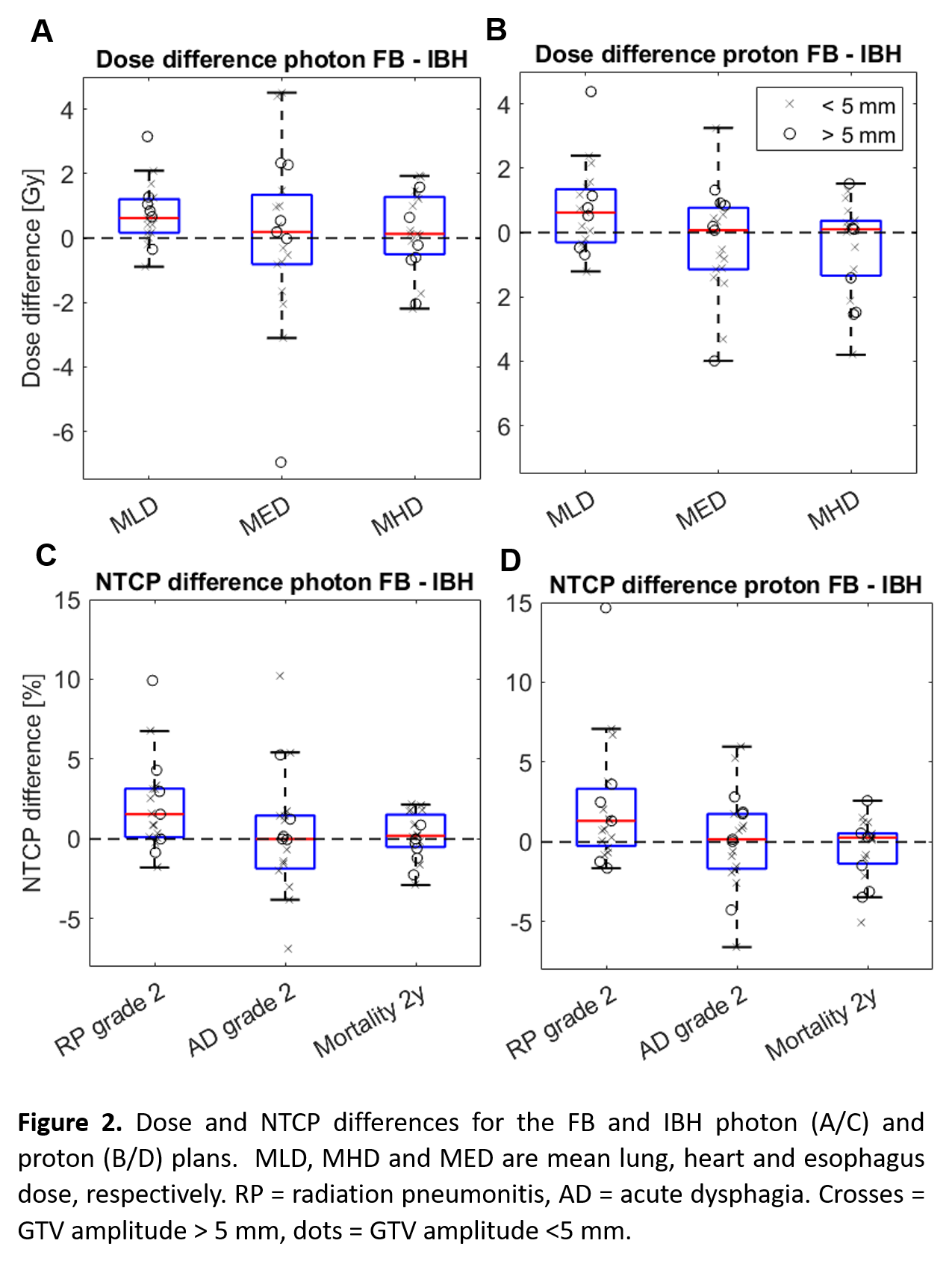
For 6/19 patients the GTV amplitude exceeded 5 mm (large movers). The GTV amplitude was 6 ± 5 mm for the entire group and 11 ± 3 mm for the large movers. Dose and volume differences are reported in Fig 1/2A/2B; NTCP differences in Fig 2C/2D. IBH slightly improved the mean lung dose (MLD) for proton and photon plans. Although statistically significant NTCP differences were seen for radiation pneumonitis ≥grade 2, the average difference FB-IBH only exceeded 5% for 2/19 photon and 3/19 proton plans. The expected 2 years-mortality decreased by >2% for 1 IBH proton plans while increasing for 4. For FB plans, 9/19 patients would have qualified for proton therapy in the Netherlands, based on the expected >2% difference in 2-years mortality, compared to 7/19 for the IBH plans.
The subgroup of large movers did not stand out in terms of IBH dose (Fig 2A,B) nor NTCP decrease (Fig 2C, D).
Conclusion
IBH did not improve relevant NTCPs for both proton and photon plans for lung cancer patients, even though for a specific subset of patients, the decrease in grade 2 radiation pneumonitis NTCP could be clinically relevant. This is in contrast with in-house results for mediastinal lymphoma patients. Further margin reduction, as well as patient or plan specific parameters that predict if a patient would benefit overall from IBH, require further investigation.
[1] Bosmans G et al., Radiother Oncol. 2006;81(1):73-80
[2] Appelt et al., Acta Oncol 2014;53(5):605-612
[3] Darby et al., NEJM 2013;368:987-998
[4] Wijsman et al., R&O 2015;117(1):49-54