Fractionated stereotactic radiation therapy for brain metastases: Outcomes and patterns of failure
PO-1303
Abstract
Fractionated stereotactic radiation therapy for brain metastases: Outcomes and patterns of failure
Authors: Nuria Farre1, Ana M. Soto-Cambres2, Saba Rabi1, Nuria Jornet3, Josep Balart1, Antoni Vila1, Jady Vivian Rojas1, Eugenia Otero1, Margarida Majem4, Ivanna Sullivan4, Andrés Barba4, Pablo Carrasco3, Gemma Sancho-Pardo1
1Hospital de la Santa Creu i Sant Pau, Radiation Oncology, Barcelona, Spain; 2Hospital del la Santa Creu i Sant Pau, Radiation Oncology, Barcelona, Spain; 3Hospital de la Santa Creu i Sant Pau, Medical Physics, Barcelona, Spain; 4Hospital de la Santa Creu i Sant Pau, Medical Oncology, Barcelona, Spain
Show Affiliations
Hide Affiliations
Purpose or Objective
To review outcomes and patterns of failure in patients treated with fractionated stereotactic radiotherapy (FSRT) for brain metastases in the setting of oligometastatic (OM) or oligoprogressive (OP) disease. Risk factors for failure in local control, disease-specific survival and brain-progression free survival were identified in a single institution retrospective study.
Material and Methods
103 brain metastases from 74 patients treated with FSRT alone or adjuvant to surgery (25%) from 2018 to 2022 were included in the study. Dose, PTV volume, tumor location, metastatic status and immune checkpoint inhibitor (ICI) treatment were collected. Kaplan-Meier method was used for survival analysis and a multivariate analysis with Cox's regression was applied to investigate the risk factors.
Results
In the studied series, 90% of primary tumors were lung cancer and 10% other types. 62% lesions were OM (≤ 5 lesions), 22% OP (≤ 5 lesions) and 16% OM brain disease in a context of polimetastatic disease before systemic treatment. 59% received concomitant, pre or post FSRT ICI treatment. Prescription doses ranged from 25 to 35 Gy, delivered in 3-8 fractions (BED10 range: 37.5-59.5 Gy). Median planning target volume was 9.6cc (range:1.1-64cc).
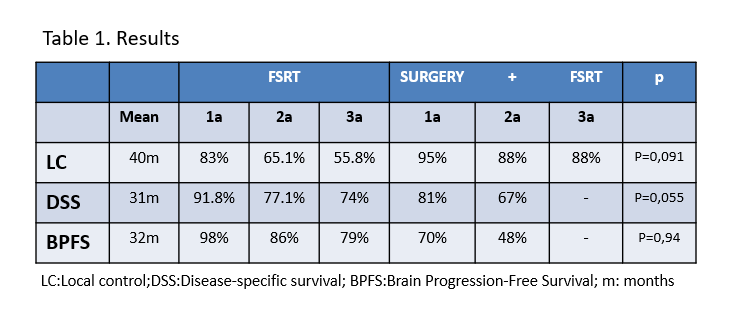
Median follow-up was 11 months (range 1-52). 1 and 2 years local control (LC) rates were 83% and 65% in FSRT alone and 95% and 88% in adjuvant FSRT, respectively. Table 1. Concomitant or pre-FSRT ICI was associated with improved local control (p= 0.013), suggesting a synergistic interaction between FSRT and ICI therapies. Disease-specific survival (DSS) at 1 and 2 years was 91.8% and 77% in FSRT alone and 81% and 67% in adjuvant FSRT. Oligoprogressive or polimetastatic status at diagnosis and infratentorial location were associated with worse DSS (p=0.025, p=0.009, p=0.035, respectively).
78% of treated patients did not develop new lesions during follow-up. Thirty new brain lesions appeared in 23 patients, 83% of them in the first year after FSRT. Median time to appearance was 5 months (range 1-28). Brain progression-free survival (BPFS) at 1 and 2 years were 98% and 86% in FSRT alone and 70% and 48% in adjuvant FSRT, respectively. Larger volumes of PTV were associated with the appearance of new brain metastases (p=0.026).
Only three lesions (2.9%) presented necrohemorragic events, one requiring surgery. Two patients had seizures (2.7%) and a cerebral edema was also observed (0.97%). No patients presented ≥ grade 3 late toxicity.
Conclusion
FSRT for brain metastases achieved a satisfactory local control and DSS with minimal risk of severe toxicity in OM and OP scenarios. Association with ICI achieves promising results in terms of local control. More than two-thirds of patients did not present new brain lesions after FSRT.