Regional Nodal Irradiation in N+Breast cancer with complete pathologic response?- Clinical practice
PO-1296
Abstract
Regional Nodal Irradiation in N+Breast cancer with complete pathologic response?- Clinical practice
Authors: Joana Pisco1, Vera Mendonça1, André Figueiredo1, Diogo Delgado1, Virgínia Mareco1, Maria Eduarda Neves1, Miguel Simas1, Manuel Carmo da Silva1, Pedro Miguel Silva1, Maria Filomena de Pina1
1Centro Hospitalar Lisboa Norte, Radiation Oncology, Lisbon, Portugal
Show Affiliations
Hide Affiliations
Purpose or Objective
Patients presenting breast cancer (BC) with clinically involved axillary nodes (AN) are often treated with neoadjuvant systemic therapy (NST). Nevertheless, when these patients have a complete pathological axillary response, the best adjuvant approach remains controversial.
Alternative axillary approaches combining sentinel lymph node biopsy (SNB) and removal of previously positive clipped nodes may avoid axillary lymph node dissection (ALND). It remains the question when it is safe and reasonable to spare ALND and/or regional nodal irradiation (RNI).
Moderate hypofractionation for whole breast and nodal irradiation has been proven to be non-inferior and equally safe compared with conventional fractionation. However, fractionation seems to differ between RT Departments, particularly regarding RNI. Our objective is to describe the practices reported by different Departments.
Material and Methods
An online survey (by Google Forms) consisting on 8 questions about the clinical vignette (vide figure) was shared through groups of Radiation Oncologists (RO) on social networks to collect data regarding target volume selection and fractionation schemes. Data was collected from the 11th February 2022, with analysis performed after data lock on the 28th June 2022. The subject was a healthy 65-years old female without any comorbidities, with a cT2cN1 luminal B-like Her2 negative invasive BC, with complete pathological response after NST, submitted to Breast Conservative Surgery and ALND.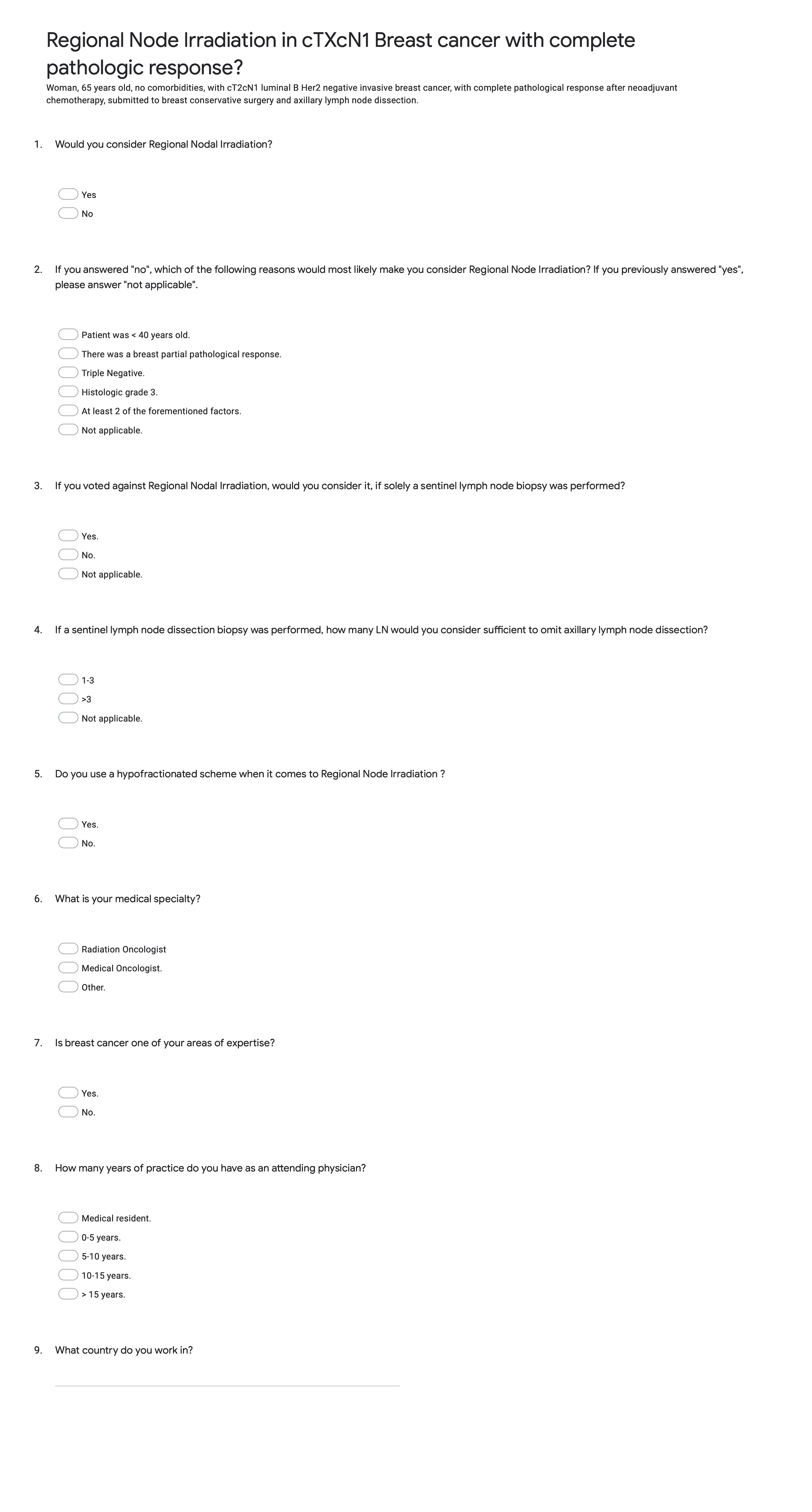
Results
In total, 241 respondents from 44 different countries completed the survey reporting their experiences. The most represented countries and groups were India 14.4%, Spain 14%, Portugal 9.8% and USA 8.9%; 76.9% were RO, 9.4% medical oncologists and 13.7% other healthcare professionals. About one third (33.6%) of the physicians had 0-5 years of practice, while 16.8% had >15 years. The minority (15.1%) were medical residents and for 77.8% BC was the area of expertise. Most would consider RNI in this patient (n = 148; 63%). Those who would not consider RNI, would change their approaches in case of breast partial pathologic response (7.7%), triple negative subtype (5.7%), patient < 40 years old (4.1%) and histological G3 (3.6%). If solely a SNB was performed, 48.3% of negative respondents would consider RNI. If a SNB was performed, 39.1% considered that >3 AN would be sufficient to omit ALND, while 40.9% considered 1-3 AN. 71.4% of respondents would consider a hypofractionated scheme for RNI.
Conclusion
Practice regarding RNI differs greatly between RT Departments, even within the same country. Most RO would consider RNI in a patient with clinically involved AN with complete pathological response after NST, especially when in presence of high risk factors, even if ALND was performed. Hypofractionated schemes for RNI are well established and can be a safe option. Trials are needed to identify which subgroups are most likely to benefit from RNI in the post NST setting.