The role of radiation therapy in patients with repeat or induced oligometastatic breast cancer
PO-1263
Abstract
The role of radiation therapy in patients with repeat or induced oligometastatic breast cancer
Authors: Ivica Ratosa1, Luca Visani2, Nika Dobnikar3, Marco Banini2, Victoria Lorenzetti2, Giulio Frosini2, Anna Peruzzi2, Icro Meattini2
1Institute of Oncology Ljubljana, Division of Radiation Oncology, Medical faculty, University of Ljubljana, Ljubljana, Slovenia; 2Radiation Oncology Unit - Oncology Department, Azienda Ospedaliero Universitaria Careggi, Department of Experimental and Clinical Biomedical Sciences "M. Serio", University of Florence, Florence, Italy; 3Institute of Oncology Ljubljana, Division of Radiation Oncology, Ljubljana, Slovenia
Show Affiliations
Hide Affiliations
Purpose or Objective
There is limited data on the role of the metastases-directed radiation therapy (MDRT) in repeat or induced oligometastatic breast cancer (OMBC). The purpose of this work is to investigate the effectiveness of MDRT (stereotactic body radiation therapy, SBRT vs. conventionally fractionated palliative radiotherapy, CFRT) in patients with OMBC.
Material and Methods
For patients with OMBC, we performed a two-institutional retrospective data collection. ESTRO EORTC classification was used to characterize oligometastatic disease (OMD) states. Primary endpoint was time to next (systemic) treatment (TTNT) as a surrogate for the duration of clinical benefit. Other outcomes included local control rate (LCR), overall survival (OS) and progression-free survival (PFS), calculated from the beginning of MDRT.
Results
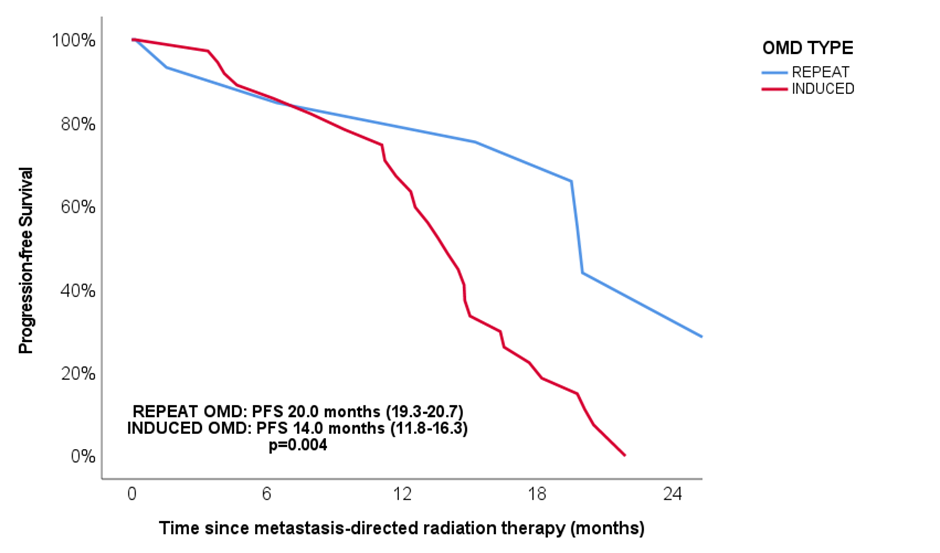
We have included 56 patients with 78 treated lesions. The median age was 60 years old (range, 39–88). Surrogate breast cancer subtypes were as follows: 37 (66.1%) hormonal positive (HR+) human epidermal growth factor receptor 2 negative (HER2-), 11 (19.6%) HR+/HER2+, five (8.9%) HR-/HER2- and three (5.4%) patients had HR-/HER2+ OMBC. Fifteen (26.8%) patients had repeat OMD and 41 (73.2%) induced OMD. OMD lesions were treated with SBRT (n=23; 41.1%) or CFRT (n=33; 58.9%). The median SBRT dose was 35 Gy (20–60) delivered in 3 (1–8) fractions and the median CFRT dose was 30 Gy (8–61), delivered in 10 (1–28) fractions. Compared to patients treated with SBRT, patients treated with CFRT reported higher rates of acute adverse events (AEs) of any grade (21.7% vs. 48.5%; p=0.038) and similar rates of G3 AEs (4.3% vs. 6.1%; p=0.675). Median follow-up post MDRT was 12.1 months (0.2–37.3). For the whole group of patients, TTNT was 7.6 months (1.6–65) and did not differ between the SBRT (6.4 months; 1.6–26.2) or CFRT groups (8.0 months; 3.5–65) (p=0.307), and between repeat (11.0 months; 2.4–26.1) or induced OMD (7.0 months; 1.6–65) (p=0.290). The median time to local progression of the OMD treated lesion was 12.5 months (2.4–51.0). One-year LCR were 100% with SBRT and 81% with CFRT (p=0.109). Overall, 30 (53.6%) patients experienced systemic progression (polymetastatic, n=17; 56.7% and oligometastatic, n=13; 43.3%). 2-year OS was 81% and median PFS was 15.1 months (12.8–17.2). Compared to patients with repeat OMD, patients with induced OMD had statistically worse PFS (Figure 1).
Conclusion
MDRT, either SBRT or CFRT, can be used to extend TTNT in patients with OMBC. Because SBRT may be more convenient for patients, it may be preferred (shorter treatment interval, better local control of treated lesions, less acute AEs). Patients with repeat OMD had better PFS.