Margin reduction while preserving coverage of axillary lymph node CTV in breast cancer IMPT
Jenneke Jacobs,
The Netherlands
MO-0392
Abstract
Margin reduction while preserving coverage of axillary lymph node CTV in breast cancer IMPT
Authors: Jenneke Jacobs1, Sophie Bosma1,2, Emmanuelle Fleury1,3, Steven Habraken1,3, Rob Louwe1
1Holland Proton Therapy Center, Radiotherapy, Delft, The Netherlands; 2The Netherlands Cancer Institute, Radiotherapy, Amsterdam, The Netherlands; 3Erasmus Medical Center, Radiotherapy, Rotterdam, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
Since 2019, proton therapy is available for selected breast cancer patients based on the model-based approach in The Netherlands. To ensure adequate target coverage, CTV-to-PTV margin of 3 mm is currently applied in addition to robust optimization to account for increased setup uncertainties of the axillary lymph node levels 1 to 4. In this study, we studied if that margin can be omitted.
Material and Methods
Ten patients treated with locoregional IMPT for breast cancer between March and August 2021 at HollandPTC were retrospectively analyzed. All patients were treated with postoperative irradiation including breast/chest wall and lymph node levels L1-2 (CTV_L1_2) and L3-4 (CTV_L3_4). In clinical practice, a 3 mm isotropic margin is applied to both CTVs in addition to robust optimization to compensate for the relatively large setup uncertainties and the impact of rotation on these volumes compared to the primary target volume.
Four different plans were created for each patient using isotropic margin expansions around CTV_L1_2 and CTV_L3_4 of 0, 1, 2, and 3 mm, respectively. For each plan, robust optimization was carried out on the expanded volumes using 21 scenarios with {5mm/3%} setup and range uncertainties. Daily CBCTs were acquired for 6D position verification and correction.
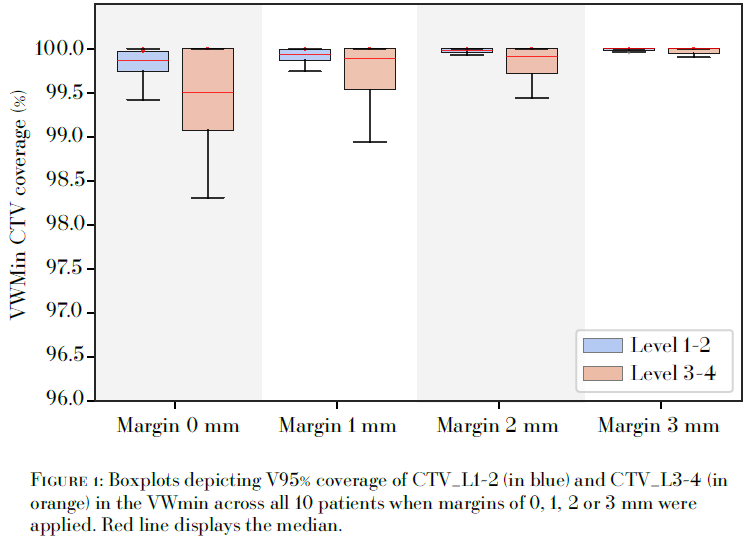
The lymph node CTVs were re-delineated on the pre-treatment CBCTs of fractions 1, 6 and 11 by a specialized radiation oncologist (CTV_L1-2* and CTV_L3-4*). After rigid registration of these CBCTs with the planning-CT (pCT), the delineated volumes were copied to the pCT. In addition, the external contour of the CBCTs were copied to the pCT and used to account for proton pathlength differences due to inter-fraction contour changes. The target coverage of CTV_L1-2* and CTV_L3-4* for the three treatment fractions was then assessed for each of the four margins using robust evaluation with 28 scenarios and {3mm/3%} residual setup and systematic range uncertainties. A minimum target coverage of 98% of the volume with 95% of the prescribed dose (V95 > 98%) in the voxel-wise minimum (VWmin) dose distribution was used as the acceptance criterion for CTV_L1-2* and CTV_L3-4*.
Results
Figure 1 shows boxplots distributions of the V95 coverage of CTV_L1-2* and CTV_L3-4* in the VWmin dose distribution across all 10 patients when margins of 0, 1, 2, or, 3 mm were applied. Overall, an increase of target coverage was observed with larger margins. However, when no additional margin was used an adequate target coverage was still observed (V95 > 98%) in 28/30 of the selected treatment fractions. For those treatment plans, a median CTV coverage of 99.87% (IQR: [99.75; 99.97%]) and 99.50% (IQR: [99.08; 100%]) was achieved to CTV_L1-2* and CTV_L3-4*, respectively.
Conclusion
Adequate coverage of the lymph node CTV levels L1-2 and L3-4 can be obtained using robust optimization based on {5mm/3%} setup and range uncertainties without additional PTV margins to compensate for larger setup uncertainties in these regions.