Evaluating intra-breath-hold variation in IMAT breast boost patients delivered in DIBH
Caroline Maguire,
United Kingdom
MO-0390
Abstract
Evaluating intra-breath-hold variation in IMAT breast boost patients delivered in DIBH
Authors: Caroline Maguire1, Syed Moinuddin2, Amanda Webster1, Rita Simoes2, Sairanne Wickers2
1University College London Hospital , Radiotherapy, London, United Kingdom; 2University College London Hospital, Radiotherapy, London, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Numerous breath-holds are performed within each fraction for deep inspiration breath-hold (DIBH) tumour bed (TB) breast boost delivery; 2 for the corrective imaging protocol (kV/kV pair clip matching), and between 2-3 for IMAT delivery. The intra-breath-hold (IBH) variation was unknown, and therefore it could not be assumed that translating the 5mm isotropic TB clinical target volume (CTV) to planning target volume (PTV) margin from the free-breathing protocol would be sufficient. The purpose of this work is to determine if a TB PTV margin of 5mm is appropriate when treating breast boost patients with IMAT in DIBH.
Material and Methods
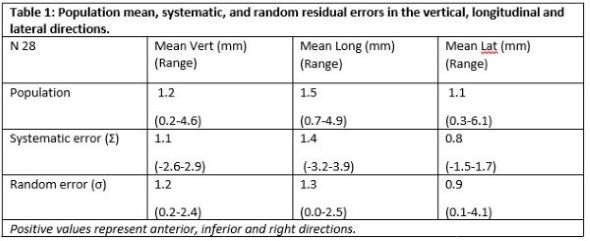
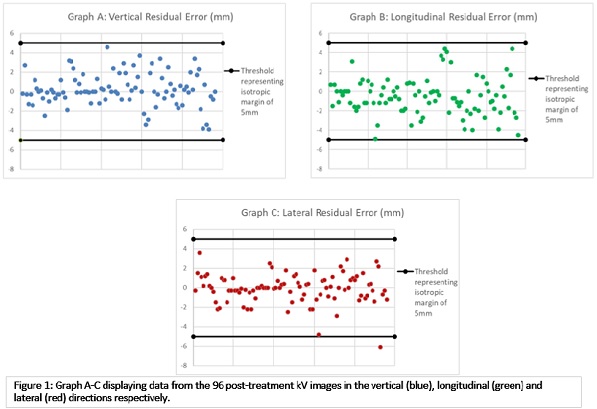
Patients with left-sided breast cancer requiring TB boost (TBB) with 12Gy in 4 fractions were prospectively identified. A 5mm TB PTV margin was applied. Residual/IBH error was quantified from post-treatment kV orthogonal paired images (according to excision cavity clip-matching). Vertical, longitudinal and lateral residual errors were determined by calculating the population mean, systematic and random errors. The Marcel Van Herk formula (2.5 Σ + 0.7 σ) was used to confirm the appropriateness of a 5mm PTV expansion.
Results
30 patients were identified between August 2020 and January 2022. This yielded 98 post-treatment kV paired images (mean 3.3 per patient, range 2-4). Two patients had only one post-treatment dataset (protocol deviation) and were excluded from the data analysis. Therefore, 96 image pairs from 28 patients are included in this analysis.
The systematic error (Σ) was 1.1mm, 1.4mm, and 0.8mm and random error (σ) was 1.2mm, 1.3mm, and 0.9mm in the vertical, longitudinal and lateral directions, respectively. Therefore, the IBH variation was <5mm, except for one outlier where the residual error was 6mm in the lateral direction for 1 post-treatment image pair (Figure 1). The Van Herk formula calculates a vertical, longitudinal and lateral TB-PTV margin of 3.6mm, 4.2mm, and 2.8 mm respectively; confirming that the IBH variation is within the 5mm margin.
Conclusion
DIBH poses an additional variable to consider when defining the TB PTV margin; IBH set-up error, as the treatment position is verified, corrected and delivered in multiple breath-holds. The resulting mean, random and systematic error must be quantified to inform the TB PTV margin. This imaging audit confirms that IBH variation is consistent, values are low and within our 5mm TB PTV margin when delivering TBB in DIBH for all tumour quadrants. This is particularly beneficial for this cohort of left-sided breast patients as heart dose is minimized. As a result, these treatments are proven to be safely delivered, and post-treatment imaging has been removed. There may be future scope based on this data to reduce the TB PTV or consider a non-isotropic margin but more patients would need to be accrued to implement a change in margins.