Impact of PTV margin reduction on organ at risk dose in short course radiotherapy of rectal cancer.
Lynsey Devlin,
United Kingdom
PO-1882
Abstract
Impact of PTV margin reduction on organ at risk dose in short course radiotherapy of rectal cancer.
Authors: Lynsey Devlin1, Sean O'Cathail2, Laura Grocutt3, Aileen Duffton1
1Beatson West of Scotland Cancer Centre, Radiotherapy, Glasgow, United Kingdom; 2Institute of Cancer Sciences, University of Glasgow, Glasgow, United Kingdom; 3Beatson West of Scotland Cancer Centre, Department of Radiotherapy Physics, Glasgow, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
For rectal cancer dose to small bowel has been shown to be
associated with acute toxicity. As PTV margin reduction results in smaller
treatment volumes, dose to organs at risk (OAR) will also decrease. There is
limited evidence of the effect of reduced PTV margins on dose to OAR in short
course radiotherapy (SCRT). Aim-To evaluate the impact of reducing PTV margins on OAR dose in SCRT
of rectal cancer.
Material and Methods
Patients
treated with SCRT between May-July 2020 were included in the analysis. A
planning CT was acquired in supine position with bowel and bladder preparation.
GTV was macroscopic tumour including rectal lumen. CTVA was GTV +
10mm margin. CTVB was elective nodes. PTV5mm, PTV 7mm
and PTV10mm were created from CTVF (CTVA + CTVB) + 5mm, + 7mm
and + 10mm respectively . OAR (bladder, small bowel loops) were delineated
as per RTOG definitions. All structures were delineated by a Clinical
Oncologist and peer reviewed by a multi-disciplinary team. For each plan the
dose prescribed to PTV was 25Gy in 5 fractions.
Treatment
plans were created using Eclipse Treatment planning system (TPS) v15.5. Three
plans were calculated for each patient with PTV5mm, PTV7mm and
PTV10mm . The same planning objectives and priorities were used
for each plan within the photon optimiser (PO) and recalculated using ACUROS
v15.5. All plans consisted of 2 VMAT full rotational arcs, 6 MV at 600 MU/min
and delivered on a Varian Truebeam (2.7) [Varian Medical Systems, Palo Alto,
Ca, USA]. Dose metrics were extracted from dose volume histograms (DVH) for all
plans.
Results
20 rectal cancer SCRT patients were
included in the analysis. Median age was 70 [IQR 60.75 -77], female (n=5), male
(n=15). Rectum level was low (n=11), mid (n=4) and upper (n= 5). A total of 60
treatment plans were analysed.
The mean volume for PTV 5mm
was 790.7 cm3 (SD 239.7), PTV7mm 930.1
cm3 (SD 267.3), PTV10mm was 1103 cm3 (SD 296.5).
The mean volume for small bowel and bladder was 206 cm3 (SD 154.5)
and 221.1 cm3 (SD 154.5) respectively. All plans complied with the planning
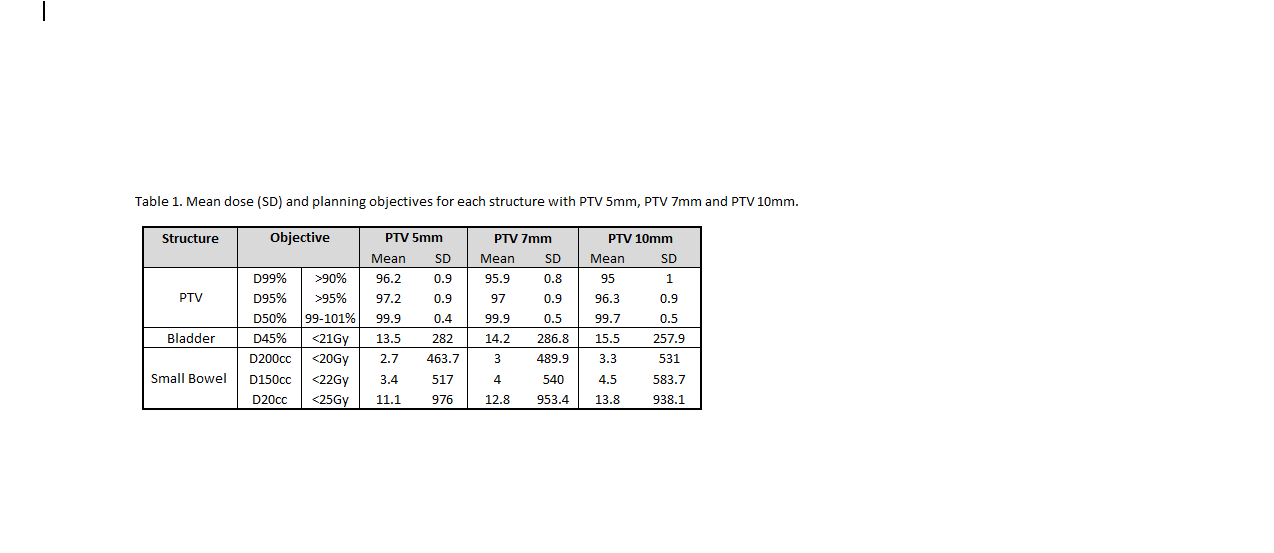
constraints for each structure (Table 1). Figure 1. Shows the population DVH for bladder
and small bowel with bladder showing most variation towards higher dose. For small bowel,
variation in dose was observed across the median volume for all PTV margins.
Conclusion
In SCRT for rectal cancer, smaller PTV
margins result in reduced dose to OAR. This is observed at the objectives and across the dose
volume histogram for this population.