NEUTROPHIL-TO-LYMPHOCYTE RATIO PREDICTS RECURRENCE AND RESPONSE IN STEREOTACTIC BRAIN RADIOTHERAPY
Fiorella Cristina Di Guglielmo,
Italy
PO-1358
Abstract
NEUTROPHIL-TO-LYMPHOCYTE RATIO PREDICTS RECURRENCE AND RESPONSE IN STEREOTACTIC BRAIN RADIOTHERAPY
Authors: Fiorella Cristina Di Guglielmo1, Marianna Trignani2, Marco Lucarelli3, Luciana Caravatta3, Annamaria Porreca4, Marta Di Nicola5, Domenico Genovesi6
1SS. Annunziata Hospital,G. D’Annunzio University, Radiation Oncology Unit, Chieti, Italy; 2SS. Annunziata Hospital, G. D’Annunzio University , Radiation Oncology Unit, Chieti, Italy; 3SS. Annunziata Hospital, G. D’Annunzio University, Radiation Oncology Unit, Chieti, Italy; 4G. D'Annunzio University of Chieti-Pescara, Department of Economics, Pescara, Italy; 5G. D'Annunzio University, Laboratory of Biostatistics, Department of Medical, Oral and Biotechnological Sciences, Chieti, Italy; 6"SS Annunziata" Hospital, "G. d'Annunzio" University, Radiation Oncology Unit, Chieti, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
Metastatic brain tumors standard of care is constantly evolving along with technological development in radiation therapy (RT) and with the identification of new prognostic and predictive factors. In the last few years, inflammatory blood markers have emerged as predictive and prognostic factors, particularly the neutrophil to lymphocyte ratio (NLR). This reflects the squilibrium between immune surveillance and tumor progression. In this scenario we aimed to assess the predictive role of NLR on early response in-field control, intracranial control and overall survival after fractionated stereotactic radiotherapy (FSRT) for brain metastases.
Material and Methods
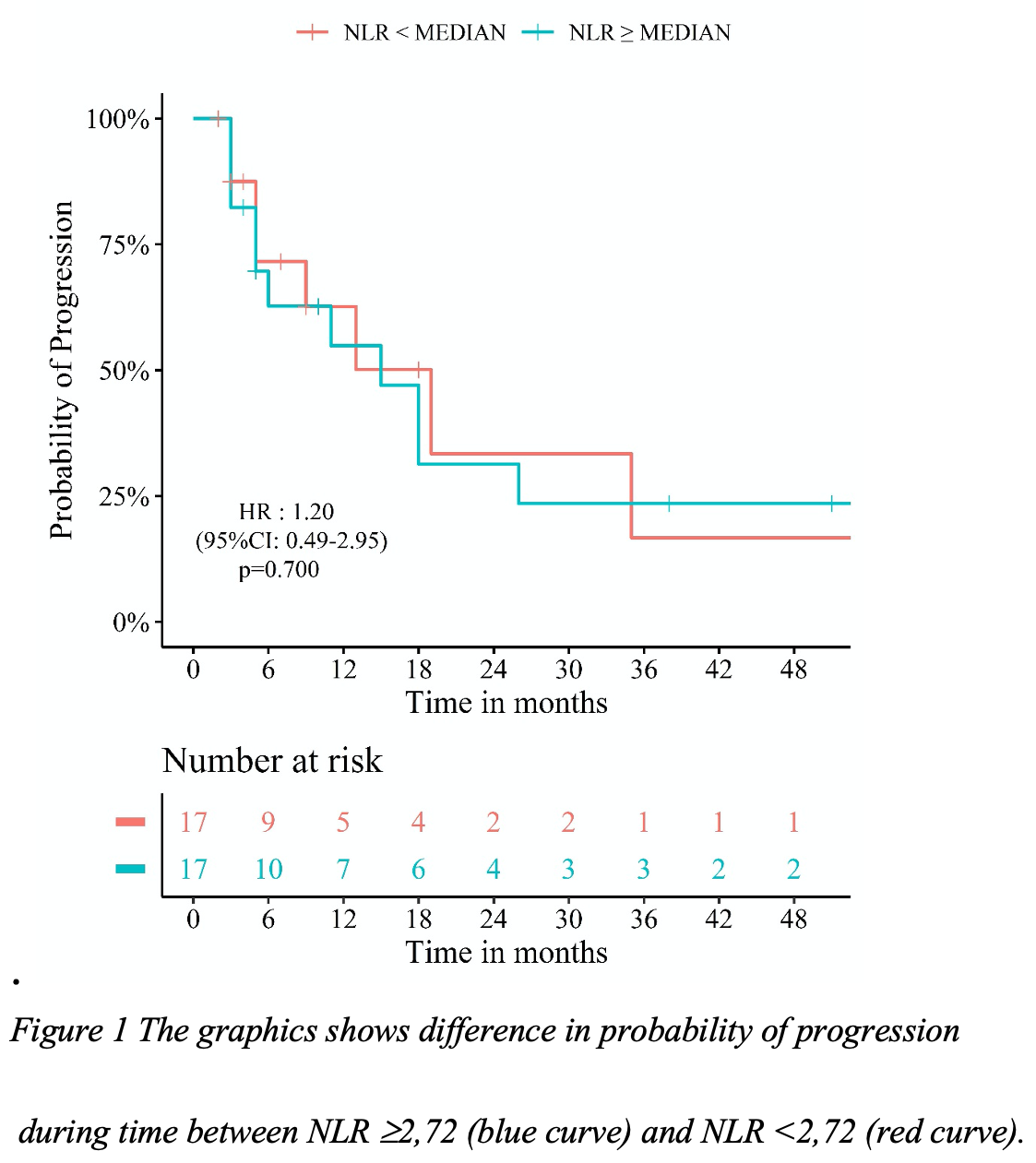
We retrospectively evaluated 34 patients with initial presentation of metastatic brain disease, treated with FSRT in our center. Laboratoristic parameters were obtained from blood count performed within one week before the start of RT. NLR, Hemoglobin and Platelets count to lymphocyte ratio were examined to establish their prognostic role respect to overall survival, disease progression and treatment response. Treatment response was evaluated with brain MRI at 3 months from the end of FSRT and then on a quarterly basis for the first two years, according to RECIST criteria. We analyzed time-to-event distributions using Kaplan-Meier's method. Kaplan-Meier curves illustrate the probability of progression in response time for patients with NLR ≥ or < MEDIAN.
Results
With a median follow-up of 14 months (3-58), a single brain metastasis (range 1-3) was treated in 74% of patients. Treatment schedules adopted ranged from 20 Gy (5 Gy/fx) to 27 Gy (9 Gy/fx). The median age was 59 years (41-81): female=20, male=14. A good Karnofsky Performance Status was detected in 88% of our sample. at the time of treatment 59% of patients was not on steroids. The median NLR value was 2.72 (IQR: 1.69 - 4.54). Patients with a NLR ≥ 2,72 showed a probability of progression 1.2 times higher than the patient with a lower value (HR 1.20; 95% CI 0.49–2.95, p = 0.700) (Figure 1). A statistically significant mean difference (p=0.012) was found for NLR between patients who had a complete response and those who did not.
Conclusion
In our study, higher values of NLR were associated with a lower response to FSRT and higher probability of disease progression. Pre-treatment immune markers of systemic inflammation have been reported as independent prognostic factors; however, the landscape is multifaceted and further validation are needed to reach the clinic.
NLR is an easily measurable, available, cost-effective parameter, useful in treatment response prediction with consequent therapeutic and follow-up strategy customization.