Systematic inflammation marker as predictor of response after neoadjuvant treatment in rectal cancer
PO-1361
Abstract
Systematic inflammation marker as predictor of response after neoadjuvant treatment in rectal cancer
Authors: Consuelo Rosa1,2, Lucrezia Gasparini1, Fiorella Cristina Di Guglielmo3, David Fasciolo1, Marzia Borgia1, Marco Lucarelli1, Luciana Caravatta1, Monica Di Tommaso1, Annamaria Porreca4, Marta Di Nicola5, Domenico Genovesi1,2
1SS. Annunziata Hospital, Department of Radiation Oncology, Chieti, Italy; 2G. D’Annunzio University, Department of Neuroscience, Imaging and Clinical Sciences, Chieti, Italy; 3SS. Annunziata Hospital, Department of Radiation Oncology, Chiti, Italy; 4G. D'Annunzio University of Chieti-Pescara, Department of Economics, Pescara, Italy; 5G. D'Annunzio University, Laboratory of Biostatistics, Department of Medical, Oral and Biotechnological Sciences, Chieti, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
Purpose: Neoadjuvant chemoradiotherapy (NCRT) followed by total mesorectal excision is a standard of care in locally advanced rectal cancer (LARC) patients. Considering the wide variation of both oncological responses and outcomes, it is currently important the possible identification of biomarkers in order to predict clinical outcomes. This aspect could allow a treatment personalization in order to obtain better responses. Our study aimed to investigate the role of haemoglobin and systematic inflammation values evaluated by neutrophil–lymphocyte ratio (NLR) and platelet–lymphocyte ratio (PLR) as possible biomarkers to predict tumor response and prognosis of LARC patients after neoadjuvant treatment.
Material and Methods
Material and Methods: We retrospectively analysed seventy LARC patients, treated with long-course NCRT and radical surgery. Pathological tumor response was evaluated according to Mandard tumor regression grade (TRG). Venous blood samples were obtained within one week before starting NCRT and during the last week of treatment. We performed a t-test analysis between independent groups to explore the prognostic impact of haemoglobin, NLR and PLR on TRG and outcomes, as local control, disease-free survival and overall survival. Post-NCRT values were also evaluated.
Results
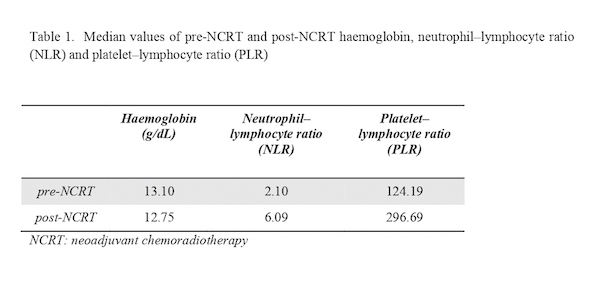
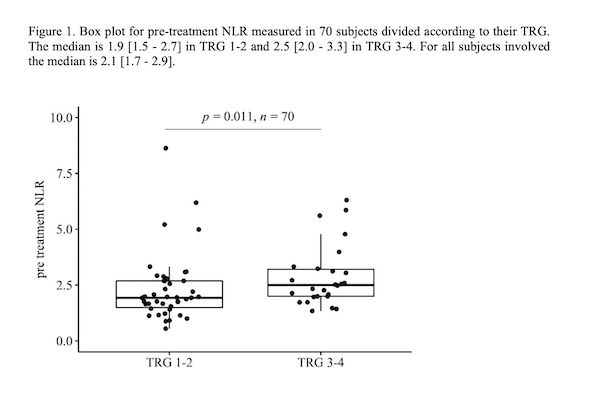
Results: Forty-four patients (62.9%) obtained a complete response (TRG 1-2). The median values of pre-NCRT haemoglobin, NLR, and PLR were 13.10g/dL, 2.10, and 124.19, respectively. The median values of post-NCRT haemoglobin, NLR, and PLR were 12.75g/dL, 6.09, and 296.69, respectively (Table 1). A statistically significant correlation between pre-treatment median value of NLR and TRG rates (p=0.011) was obtained with values of 1.9 (range: 1.5-2.7) in TRG 1-2 versus 2.5 (range: 2.0-3.3) in TRG 3-4 (Figure 1). Besides, no statistically significant correlations were found for pre-NCRT haemoglobin value and PLR with TRG 1-2 versus TRG 3-4 (p= 0.930 and p=0.710, respectively). Furthermore, no significant correlation was obtained between pre-NCTR values and clinical outcomes. We also evaluated post-NCRT blood values but none of them resulted in a significant correlation with TRG neither outcomes.
Conclusion
Conclusion: The prognostic significance of systematic inflammation values, as haemoglobin, NLR and PLR, is an interesting argument and it has been explored in several neoplasms. In our study a higher (2.0 - 3.3) pre-NCRT NLR resulted as a predictor of poor pathological tumor response. The study is still ongoing in order to be validated in a larger number of patients. This could be helpful to define predictive models for treatments personalization, allowing the possibility of an intensified therapy, especially in poor-responders’ patients.